Post operative Dry Eye
Introduction
Over the last decade there has been a increased incidence of anterior segment eye surgeries being performed across both the public and private sector. Anterior segment surgeries include procedures such as; cataract surgery, corneal transplantation, microinvasive glaucoma surgery (MIGS) and laser refractive surgery.
The exact number of cataract surgeries globally can vary significantly due to differences in healthcare systems, access to care, and reporting practices. Estimates suggest that cataract extraction is performed approximately; 3.7 million cases per year in the USA; 7 million cases per year in Europe and 20 million cases per year worldwide1. Demand for cataract surgery is expected to continue growing in the coming years2,3 due to an aging population and increased life expectancy. In addition, advances in technology and surgical techniques may improve outcomes and increase the attractiveness of both lens based and laser refractive surgeries.
Common invasive anterior segment procedures include:
Corneal surgery
- Lenticule Extraction e.g. SMILE
- LASIK
- Keratoplasty (DMEK/DSEK/DALK/PKP)
Cataract Surgery
- Clear Lens Extraction (CLE)
There is clear evidence that dry eye disease (DED) can be exacerbated by these procedures4,5, and this can result in ongoing patient discomfort and dissatisfaction with the procedure. Because of this there are a number of patients whose quality of life (QOL) is adversely affected to a significant degree.
While most of the research and technological advancements in eye care focus on improving outcomes and preventing serious vision problems, it is important not to forget about the less severe side effects, even though they’re not sight threatening.
The impact of DED goes beyond the patients’ post-operative experience. It’s also a key factor in a clinic achieving accuracy in cataract and refractive surgery. Accurate topography, tonometry, and biometric measurements are essential for surgical planning and great post-op vision6,7. It is well acknowledged that a healthy, intact pre-corneal tear film8 is required as it is the eye’s first refractive component. Therefore, to maximise accuracy a complete pre-op assessment for surgery should also include a comprehensive screen for DED.
There are a few steps listed below that take place as part of the surgical pathway that will cause or exacerbate existing dry eye. These steps are necessary e.g. using antiseptic eyedrops pre-op to reduce the risk of infection, but the clinical team should be aware of the potential impact on the ocular surface.
- Repeated drying/irrigationDuring cataract surgery, the eye’s surface is exposed and goes through cycles of drying and irrigation to keep things clear for the surgery. This can potentially harm the corneal and conjunctival surfaces.9, 10 The use of an ophthalmic visco-surgical device (OVD) during the procedure coats the ocular surface and has been shown to significantly improve TBUT, OSDI scores and ocular surface staining 1 week post-operatively.11
- Intra operative drops
– Iodine/Povidone
– Anaesthetics
– Non-steroidal anti-inflammatory drops (NSAIDS)
– Preservatives in eye drops e.g. benzalkonium chloride (BAK)Ocular surface damage may be due to the toxic effects of eye drops. The use of eye drops during and after surgery may lead to potentially harmful effects on the ocular surface with injury to corneal epithelial and conjunctival epithelial and goblet cells.12
Using povidone-iodine just before surgery is excellent for reducing the risk of post-operative endophthalmitis,13 but studies have shown it can be toxic to the corneal surface14, 15 The same goes for topical anaesthetic drops which can cause similar issues.16, 17 So, it’s important to carefully choose the type and amount of these drops, especially for patients with existing dry eye or other eye surface diseases. After routine cataract surgery, patients usually get a mix of steroid, anti-inflammatory, and antibiotic drops as part of their care. These drops often have preservatives, which studies have found can be harmful to the ocular surface. 18, 19
- Photo toxicity form lamps and microscope
Studies have shown that the light from the operating microscope can have phototoxic effects on the eye’s surface.20-22 It’s still unclear how much this phototoxicity, along with factors like the drying of the eye during surgery and the need for frequent irrigation, contribute to dry eye disease (DED) after cataract surgery. This needs more research, with a focus on each factor individually. In the meantime, for patients at risk of DED after cataract surgery, it’s a good idea to limit the exposure to the operating light as much as possible to avoid eye surface damage and potential DED-related issues. - Surgical Trauma
– Speculum
– Opening Femtosecond Laser (FL) Incisions
– Femtosecond Laser-assisted Cataract surgery (FLACS) Suction RingCorneal nerve damage can occur intra operatively in surgery such as LASIK, PRK and cataract surgery. This can affect the radial stromal nerves, particularly in full thickness wounds in cataract surgery. The result of this can lead to a disruption of tear film homeostasis.23
Over the years various studies have shown that cornel nerve function is reduced post cataract surgery and may still be reduced up to 3 months after the operation.24 Patients are warned of this loss of sensation pre-operatively along with the potential exacerbation of DED that may result after the procedure. Surgical trauma can also arise from the use of the speculum intra operatively, femtosecond laser (FL) incisions, and femtosecond laser assisted cataract surgery (FLACS) suction rings may lead to ocular surface damage which can include the corneal epithelium and the conjunctival epithelial goblet cells as well as corneal nerves as already mentioned
The incidence of dry eye post cataract surgery varies widely in the literature and ranges from 9% to 100% in different studies depending on clinical markers.12 Ishrat et al. reported clinical signs of DED in 9% of patients 4 weeks after surgery.5 On the other hand, Miyake and Yokoi documented such problems in 31% of patients at the same time period.25 Interestingly in a prospective study of 100 patients, Dasgupta and Gupta found that at 12 weeks post-surgery, 100% of patients had a tear break up time (TBUT) abnormality.16 Helpful diagnostic and treatment algorithms, such as the ASCRS Preoperative OSD Algorithm27 have been proposed to help identify pre-existing dry eye and management algorithm to maximise refractive accuracy and patient comfort through the surgical journey.
Clinical Evaluation
A thorough pre operative history and examination remains the most effective tool in identifying DED and thus altering the patients journey through surgery.
Risk Factors
Pre-existing Dry Eye – If patients already have dry eye (maybe not fully or correctly identified before surgery), it can affect their vision quality and may adversely affect refractive measurements before eye surgeries such as keratorefractive and phacorefractive procedures.27
Symptoms
These may vary greatly from patients who are asymptomatic to those who have severe symptoms. Very often there is poor correlation between signs and symptoms.
Signs
Examination should be comprehensive using the “Look, Lift, Pull, Push” approach which assesses the full ocular surface and adnexa and can be complemented by invasive (Corneal staining, Corneal sensitivity testing, osmolarity testing, Schirmers testing, MMP-9) and non invasive (Meibography, topography, Non Invasive – Tear Break Up Time, OCT Tear Meniscus height, OSI) tests.
Examples of important clinical signs and significant test results include (College of Optometrists, 2022)28
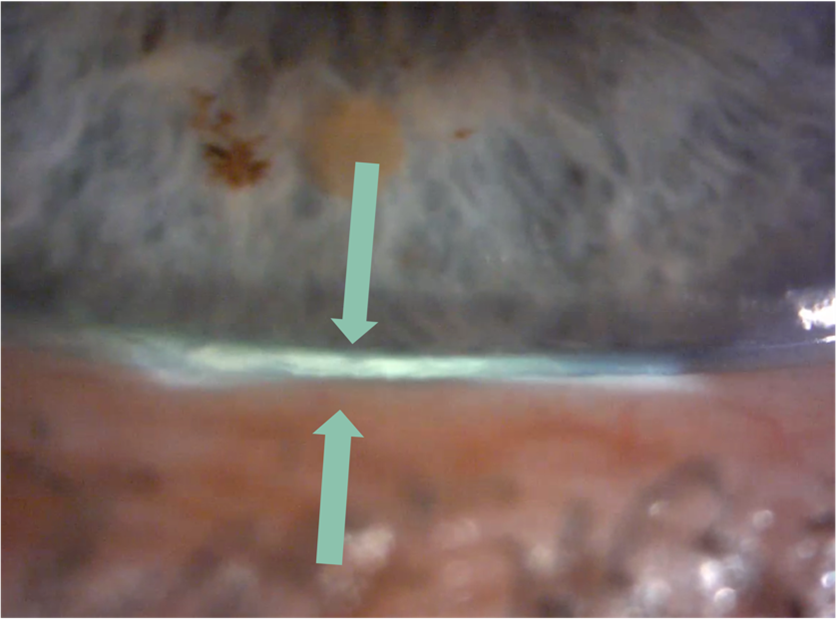
- Reduced tear meniscus at inferior lid margin (following the instillation of fluorescein, normal meniscus is not less than 0.2 mm in height)
- Raised tear osmolarity (308 mOsm/l is the most sensitive threshold to distinguish normal from mild/moderate DED, while 315 mOsm/l is the most specific cut-off)
- NITBUT <15s
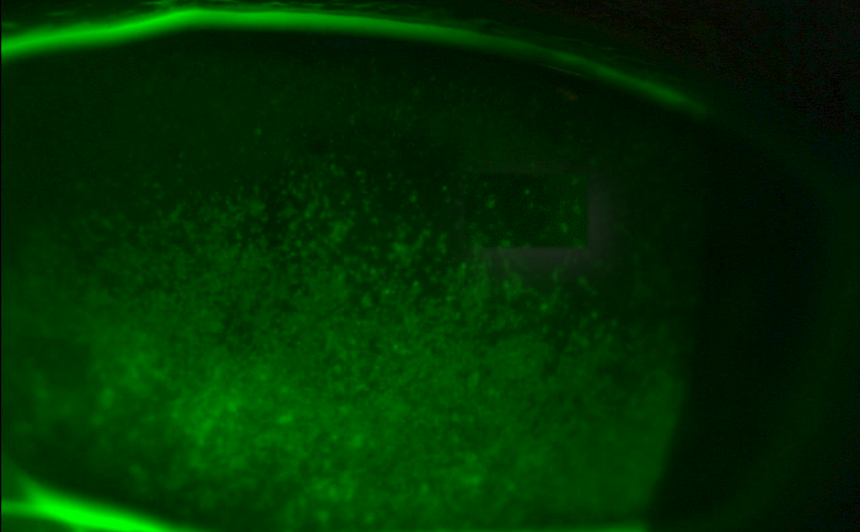
- Fluorescein break-up time (FBUT) <10 sec
- Schirmer test (without anaesthesia) ≤ 5mm in 5 min; may be helpful in the diagnosis of Sjögren’s Syndrome, but of limited value in non-Sjögren’s DED
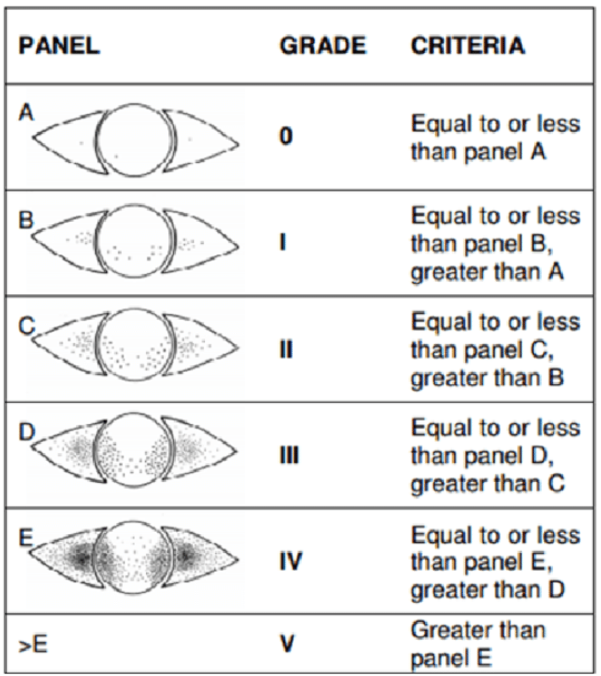
- Punctate epithelial erosions in exposed area of cornea and bulbar conjunctiva (especially in inferior third of palpebral aperture). Stain with vital dye(s) as available. Various grading systems are available (e.g. Oxford staining score)
- Lid wiper epitheliopathy
- Increased mucus strands and other tear film debris
- Filaments (adherent comma-shaped mucus strands)
- Mucus plaques
- Dellen
- Thinning and (very rarely) perforation
- Reduced corneal sensitivity
Management and Advice
The main aim of management is to reduce and optimise DED at each stage of the surgical journey.
Pre-operative management
It’s really important to diagnose and manage any existing DED before cataract surgery. Tear film irregularities can lead to inaccurate biometric and corneal topographic assessments5, and the problem can get worse after surgery. So, taking care of DED beforehand is crucial.
Intra-operatively
As mentioned earlier, several factors during cataract surgery can contribute to surgery-induced DED. These include corneal nerve damage from surgical incisions, the toxic effects of povidone-iodine and anaesthetic drops, repeated drying and irrigation of the eye surface, phototoxicity, and direct trauma to the eye surface. Cataract surgeons need to be aware of these risks, especially when operating on patients who already have DED. Reduced volumes of topical anaesthetic, care with speculum insertion and use of dispersive OVD can help protect the ocular surface during the surgical period. Trying to avoid incisional approaches for astigmatism can also reduce corneal nerve damage.
Post operatively
After cataract surgery, it’s standard practice for patients to use topical steroid, non-steroidal anti-inflammatory, and antibiotic drops for approximately 1 month, with preservative free being preferred to improve TBUT and OSDI scores. 29 In addition, patients may also be given lubricating eye drops, topical cyclosporin drops, mucin secretagogues, anti-inflammatory agents such as topical lifitegrast, omega 3 supplementation, lactoferrin, lid wipes, and bandage contact lenses.
These are summarised in the table below by Naderi et al. 24
Pre-operative | Intra-operative | Post-operative |
Assess for DED | Limit incisional damage | Assess for DED |
Assess for OSD | Micro-incisional surgery | Avoid XS drop regimens |
Consider PF drops | Consider avoiding AKs with DED/OSD | Consider PF drops |
DED/MGD | Limit drop exposure | Lubricating drops/ointment |
Avoid XS topical anaesthetic application | Management of MGD – Lid hygiene – Tea tree oil – Omega III – Topical Azithromycin – Systemic tetracycline | |
Single pre-op. drop of Povidine 5% | Topical Cyclosporin – Other anti-inflammatories – Lifitegrast | |
Care with pre-op NSAIDS in those with DED | Mucin Secretagogues | |
PF drops in those with DED/OSD | Care with NSAIDs – Avoid with DED | |
Limit repeated drying/irrigation | Punctal Plugs | |
Consider coating OS with dispersive OVD – All those with DED – As a routine | ||
Limit surgical time where possible | ||
Limit Phototoxicity | ||
Reduce surgical time/exposure | ||
Microscope illumination – Adequate not excessive | ||
Limit surgical trauma | ||
Careful insertion of speculum | ||
Care with FLACS suction ring | ||
Avoid epithelial trauma | ||
Opening FLACS incisions | ||
Limit holding eye with forceps |
AK = Arcuate keratotomy
DED: dry eye disease; MGD: Meibomian Gland Dysfunction; OSD: Ocular surface disease; NSAIDs: Non-steroidal Anti-inflammatory drugs; FLACS: Femtosecond laser-assisted cataract surgery; OVD: Ophthalmic Viscosurgical Device; XS: Excess; PF: Preservative Free; OS: Ocular Surface.
This article serves as an overview of the condition and treatment options. It does not serve as a clinical guidance. Eyecare provider guidelines should be used when managing patients.