Meibomian Gland Dysfunction
Introduction
The meibomian glands in the eyelids, which synthesize and secrete lipids for the superficial tear film layer (i.e the lipid layer), play an important role in maintaining a healthy ocular surface through reducing tear evaporation. However, dysfunction of these glands, known as meibomian gland dysfunction (MGD), is the leading cause of evaporative dry eye disease and is one of the most common conditions encountered by eye care providers.1 The literature indicates that over 80% of patients with dry eye have MGD as a primary or contributory cause of DED. 2-4 In addition, MGD is an ever-increasing problem and it is estimated that 69% of people over the age of 40 years will have some degree of MGD and this only increases with age.
The most used definition of MGD from the International Workshop on Meibomian Gland Dysfunction is that it is:
A chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/ quantitative changes in the glandular secretion. This may result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease 2
Several forms of MGD are differentiated, such as hyposecretory and hypersecretory forms, with subdifferentiation into primary and secondary diseases. All forms of MGD eventually lead to increased evaporation of the tear film. Other associated systemic diseases include the following: atopy, acne rosacea, seborrheic dermatitis, and cicatricial pemphigoid, along with ageing processes and drug side-effects.2
The meibomian glands are located on the upper and lower tarsal plates. There are approximately 25-40 meibomian glands in the top eyelid and 20-30 meibomian glands in the bottom eyelid. They are responsible for producing the top oily layer of the tear film, called meibum which stops the tears evaporating. The meibomian secretion (meibum) is a complex mixture of cholesterol, wax and cholesteryl esters, phospholipids with small amounts of triglycerides and triacylglycerols, and hydrocarbons.2 Each meibomian gland has a central duct with small sacs attached to it called acinus. Meibum is released in a process by which:
- Lipid is synthesized in the acinus constantly
- The acinus internal cells known as the acini burst which forces the meibum into the central duct.
- As more meibum continues to be produced and pushed into the central duct this forces it closer to the terminal duct.
- Blinking creates a pressure which forces the meibum into the terminal duct and out onto the eyelid.
It is theorised that the reason glands die and drop out is due to the increased pressure that can build up inside the gland. Normally that pressure (when blinking) is used to express the meibum out of the gland and onto the eye surface, forming the top layer of the tear film. If the gland is blocked by overly thick meibum, then this expression is hindered, and there is a back log of excess meibum which increases the pressure in the chambers of the gland (acini). Over time this pressure means that the acini cells are not able to be nourished and waste products removed efficiently so they eventually die. When enough cells have died, the gland will stop working – this is referred to as meibomian gland drop out.
Using meibography technology, previous studies have discovered that meibomian gland dropout can be affected by various factors, including age, contact lens wear, the use of antiglaucoma eye drops, Sjogren’s syndrome (SS), and graft-versus-host disease (GVHD). More recent findings show that intensive, compared to less frequent, computer users generally have greater meibomian gland drop out.5 Once the glands die and drop out, they cannot be replaced and so the function of the glands as a group will only decline over time and the best outcome that can be hoped for is to slow down or stop the deterioration in function however, it will not be reversed. It is therefore crucial that MGD is picked up as early as possible and treated as aggressively as required to provide the best possible outcome for the patient. The goal of treatment for MGD is to improve the flow of meibomian gland secretions, by improving the quality or quantity of meibum expressed, and ultimately help re-establish tear film stability.1
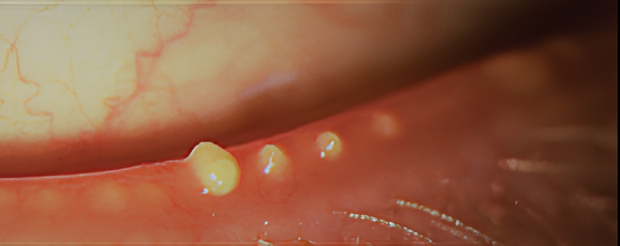
- Normal: In the normal meibomian gland, the secretory product (meibum, yellow arrows) that is produced inside the acini is transported through the connecting ductules into the central duct and is finally delivered through the excretory duct and orifice that is located within the keratinized epidermis (red) at the posterior lid border. The ductal system has an incipient stage of keratinization (pink). The acini are spherical to elongated, and the connecting ductules are narrow.
- Obstruction
- Additional dilatation: The continuing secretion of meibum in the acini generates an increasing pressure inside the glands that leads to a gradual dilatation, first of the central duct.
- Additional atrophy: After a prolonged time, the increased pressure inside the gland leads to dilatation of the connecting ductules and a pressure atrophy of the acini with rarefaction of secretory meibocytes. This effect causes shrinkage of the whole acini that may represent the histopathologic equivalent of the clinically detectable gland dropout and results in a presumed secondary hyposecretion.
- Additional cornification of the glandular epithelium: In late stages the whole ductal epithelium can become cornified and the meibocytes replaced by a stratified squamous cornified epithelium.
Clinical Evaluation
Risk Factors
- Increasing age
- Asian ethnicity
- Postmenopausal hormonal therapy
- Poor diet in relation to the balance between omega-3 and omega-6 fatty acids.
- Environmental factors such as increased screen use
- Contact lens wear
- Systemic conditions such as Sjörgens syndrome.
Signs
The following three parameters are the most commonly used methods to evaluate the morphological characteristics and function of meibomian glands in clinical practice: abnormalities of lid margins, expression of meibum, and gland dropout degree visualized by meibography.
- Blocked/capped meibomian glands
- Notching of lid margin/meibomian gland drop-out
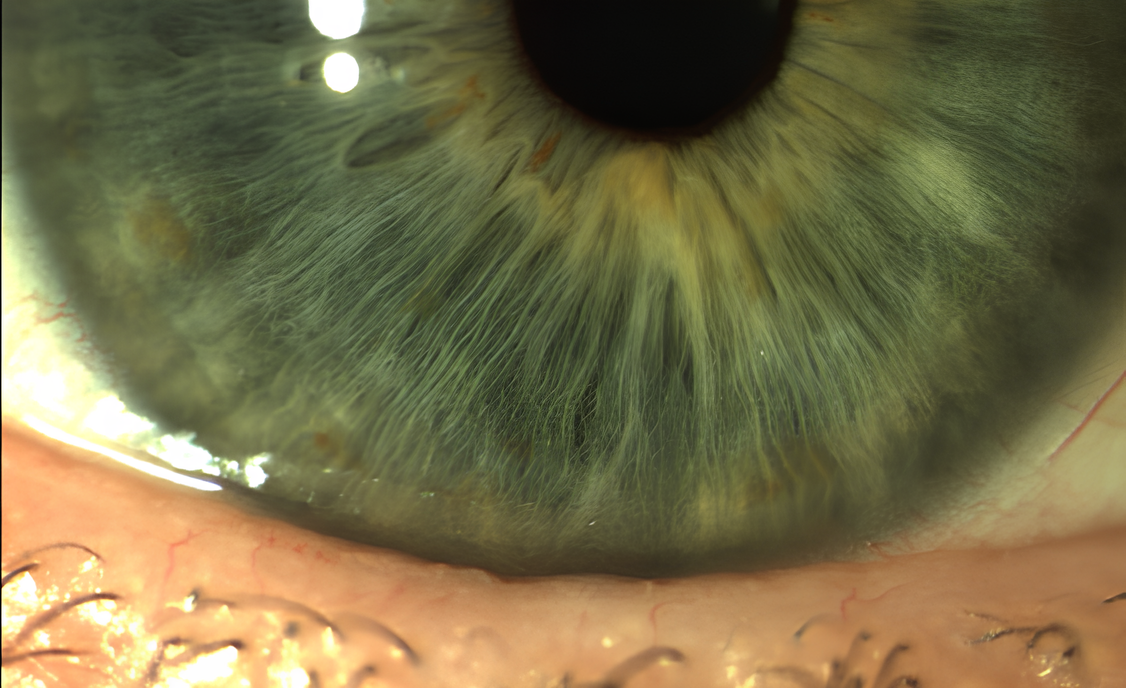
- Telangiectasia
- Keratinised gland openings
- Inflammation of posterior lid margin
- Vascularised lid margin
- Lash loss
Symptoms
- Redness
- Itching/irritation
- Burning eyes
- Watery eyes
- Photophobia
- Foreign body sensation
- Intermittent blurry vision
The Efron scales are commonly used in clinical practice to grade the severity of MGD and provide guidance on treatment.
Management & Advice
There is no gold standard treatment for meibomian gland dysfunction, but rather a diversity of options.1 The goal of all MGD treatments is to improve the flow of the meibum, leading to a more stable tear film.6 There is a range of treatment options available for the management of MGD that are non-pharmcological treatments including warm compresses, cleansing agents, lubricant drops, and essential fatty acid supplementation; medical treatments including antibiotics, non-steroidal and steroidal anti-inflammatory agents, hormone therapy; control of Demodex infestation and procedures including, gland expression, intraductal meibomian gland probing, the use of electronic heating devices, intense pulsed light therapy, and intranasal neurostimulation.
Non-Pharmacological Treatments
Warm Compresses: Due to many factors as listed above the meibum may be of poor quality or obstructed. It is therefore necessary to use heat to liquify the meibum to allow it to be expressed more freely. Evidence suggests that the melting point of meibum is between 32°C-45°C,2 the poorer the quality, or the more the obstruction the higher the melting point will be within the range of 32°C-45°C.2
Older versions of the warm compress would be a warm face cloth over the eyelids; however, we now know that this would mean the heat would dissipate very quickly and to improve the quality of the meibum you need consistent heat of a temperature of ≥40°C.8,9 Studies have shown that comparing a warm face cloth and a heat mask, a face cloth has no effect on the MGD however, the heat mask reduces the MGD. 8
After the heat is applied, it is recommended to express the glands by form of gentle massage.7 The international workshop on MGD recommends that “patients may be told that after application of a hot compress to the eyelids, they should apply traction on the lateral canthus to immobilize the upper and lower eyelids; that should be followed by down- or upward mild compression of the eyelids with the finger of the opposite hand beginning at the nasal canthus and moving laterally toward the lateral canthus”.7
Eyelid Hygiene: Because of the close proximity of the eyelashes to the meibomian glands disorders of one can affect both.9 It has been reported that ecto-parasites demodex folliculorum (DF) tend to live in the eyelash follicles and demodex brevis (DB) tend to burrow into the meibomian glands and are associated with MGD. 9 Treatment is needed to reduce the quantity of DB and DF which has shown to improve patient symptoms and ocular surface health. 9
It has been found that high heat especially ≥40°C causes protein coagulation and denaturation and paralysis of the DF nervous system. This is where warm compresses are useful. It is useful to note that heat masks come in a moist or a dry heat. It has been reported that moist heat helps to soften the eyelash debris in anterior blepharitis.9
It is recommended that patients use an eyelid cleanser (e.g. eyelid wipes, eyelid gel or cleansing solution) to remove debris and create a clean periocular environment.
Lubrication: Preservative free eye drops have shown greater effectiveness than preserved drops in decreasing inflammation on the ocular surface and increasing the antioxidant contents in tears of patients with DED.10 Drops should be recommended at the end of the regime to restabilise the tear film. There are specific drops that can help address the compromised lipid layer by adding lipids to the ocular surface or by helping the lipids that are present work more effectively to create a working lipid layer.
Omega 3 Supplementation: Omega-3 fatty acid supplementation is a potential management option for MGD due to its anti-inflammatory properties and influence on meibum health.13
- Anti-Inflammatory Effects: Omega-3 fatty acids reduce inflammation in the eyelids, addressing the root cause of MGD by improving the function of the meibomian glands, which produce the oily component of tears.
- Modulation of Meibum Composition: Omega-3s may alter the composition of meibum, making it less viscous and more fluid. This modulation prevents blockages in the meibomian glands, enhancing tear quality and reducing symptoms.
- Stabilization of Tear Film: By improving the quality of meibum, omega-3 supplementation stabilizes the tear film, preventing excessive tear evaporation and reducing symptoms of dry eye.
- Reduction of Dry Eye Symptoms: Omega-3 supplements have been shown to alleviate symptoms of dry eye, including dryness, burning, and blurred vision, commonly associated with MGD.
- Potential Improvement in Gland Function: Some studies suggest that omega-3 supplementation may enhance the function of meibomian glands over time, providing long-term benefits for managing MGD and associated dry eye symptoms.
Pharmacological Treatments
In some cases, topical ophthalmic medications such as corticosteroids or antibiotics (eg azithromycin) may be considered. Azithromycin has anti-inflammatory effects and has been shown to improve signs of eyelid disease. Weak topical corticosteroids may also be prescribed and while these drugs don’t directly act on the meibomian glands, they do reduce eyelid inflammation. A short course of these is to be considered by clinicians due to their ocular side effects. Systemic azithromycin has also emerged as another alternative. The benefits to this management option being that it can be prescribed over a shorter timeframe, and it has a better safety profile with less side effects. In a recent study comparing systemic doxycycline and topical azithromycin it was found that topical azithromycin was more effective in improving the quality of the tear film and having fewer side effects, better compliance and better tolerability.12
Systemic antibiotics can be an effective second line management option for some patients. In this case it is the anti-inflammatory action of the antibiotic that is thought to be effective rather than anti-infective.11 The main class of antibiotics traditionally used were tetracyclines such as oxytetracycline, doxycycline, minocycline, or lymecycline. These are generally prescribed at a lower dose than normal, and treatment may need to be over the course of several months. Clinicians are advised to check on their local guidance for more details on this. Where tetracycline type antibiotics are used clinicians should note that they are contraindicated in pregnancy and lactation, and there are side effects which patients should be warned of such as photosensitivity and skin rashes as well as upset stomach. Where tetracyclines are contraindicated erythromycin may be considered.
Procedures
Many clinicians consider using devices that help melt and express meibum including LipiFlow Thermal Pulsation System, MiBo Thermaflow and Intense Pulsed Light treatment (IPL). The principal function of LipiFlow Thermal Pulsation System and MiBo Thermaflow is to provide heat to melt meibum and promote gland function. These treatments last 12-15 minutes per eye. IPL treatment focuses on abnormal blood vessels in the eyelids linked to inflammation and meibomian gland obstruction, addressing chronic inflammation and gland blockage. IPL pulses generate heat energy that penetrates the skin, reaching deeper structures like the meibomian glands. This heat liquefies and releases thickened, obstructed meibum, improving gland function and may also stimulate collagen production. These procedures are often combined with other MGD treatments such as eyelid hygiene, warm compresses, lubricating eye drops, and omega-3 supplements to optimise results and provide comprehensive management of MGD.
This article serves as an overview of the condition and treatment options. It does not serve as a clinical guidance. Eyecare provider guidelines should be used when managing patients.