Tolosa-Hunt Syndrome and tuberculosis: a diagnostic and management challenge
Patent presentation
32-year-old lady presented to eye casualty with a four-day history of left eye (LE) pain, reduction in vision (acuity and colour) and diplopia͘. Her past medical history included two previous episodes of Bell’s Palsy and a recent tooth extraction͘. She was originally from Mozambique before moving to Portugal and then to the United Kingdom 6 years ago͘. On examination, there was a left sided relative afferent pupillary defect with a reduced visual acuity (V ) to hand movement in the LE. She demonstrated painful ophthalmoplegia with limited abduction, adduction, and elevation of her LE with a 3mm proptosis͘. There was neither periorbital oedema nor erythema, but mild left sided optic disc swelling was elicited͘. B-scan ultrasound showed no evidence of posterior scleritis͘. Blood results demonstrated a mildly elevated C-Reactive Protein of 13mg/L Thyroid function tests were normal͘.
Autoimmune screen including serum angiotensin converting enzyme was negative͘. Chest X-ray was clear with no hilar lymphadenopathy. Infective screen for HIV, syphilis and Mantoux test were also negative.
Computerised tomography (CT) of her head and orbit showed localised thickening and enhancement of the bulk of the left medial rectus muscle extending posteriorly to the orbital apex. No compressive lesion or abnormal enhancement was seen at the orbital apex or in the region of the cavernous sinus͘. Left optic nerve appeared slightly bulky although no abnormal enhancement was seen͘. Subsequent magnetic resonance imaging (MRI) of the head and orbit largely concurred with the CT findings, although a small area of low signal close to the left cavernous sinus was described in post-contrast images, which was attributed to partial volume effect with no large enhancing component. She was treated with a three-day course of intravenous methylprednisolone and then a tapering course of oral Prednisolone presumed diagnosis of idiopathic orbital inflammation was made as she had shown marked improvement with steroids.
Five years later, she presented with a recurrence of diplopia and painful ophthalmoplegia in the LE. Exploring further history revealed that prior to current presentation, she had repeated episodes of similar symptoms which improved significantly with tapering course of systemic steroids͘ V was 6/9 in the right eye (RE) and 6/12 in the LE. There was no relative afferent pupillary defect and no anisocoria Ishihara colour vision was normal in both eyes. Left eye conjunctiva was hyperaemic but there was no evidence of keratitis or uveitis. Dilated fundus examination did not reveal any abnormality.
Diagnostic testing
CT orbit demonstrated a left sided soft tissue mass within the cavernous sinus (Figure 1), with subsequent MRI head and orbit confirming this as an avidly enhancing mass in the left cavernous sinus measuring 22mm x 7mm, extending into the orbital apex but with no intra-orbital extension (Figure 2a & 2b)͘. The left optic nerve was not compressed.
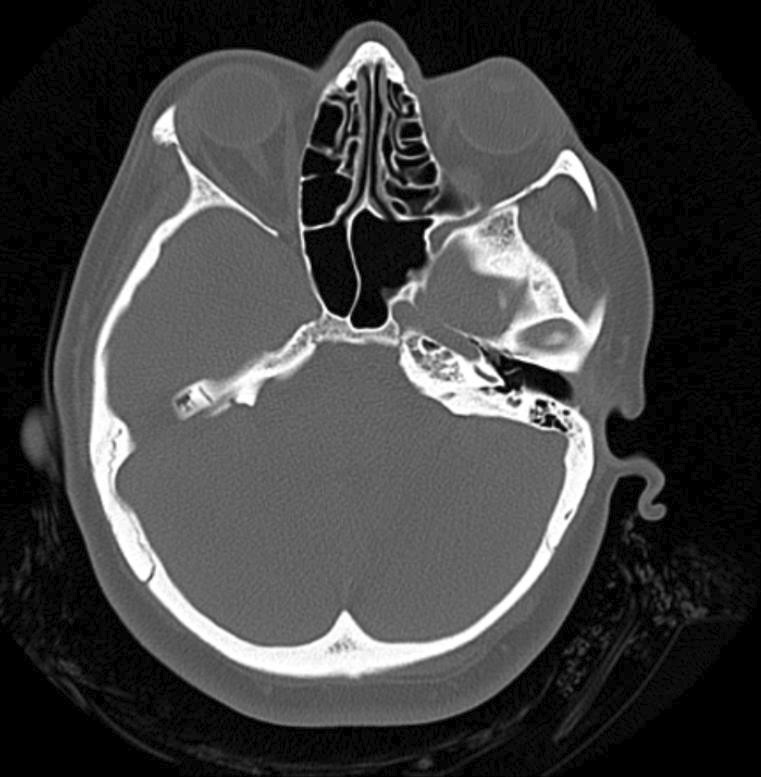
Figure 1: Computerised tomography (CT) scan of the orbit (axial cut) showing a left sided soft tissue mass within the cavernous sinus.
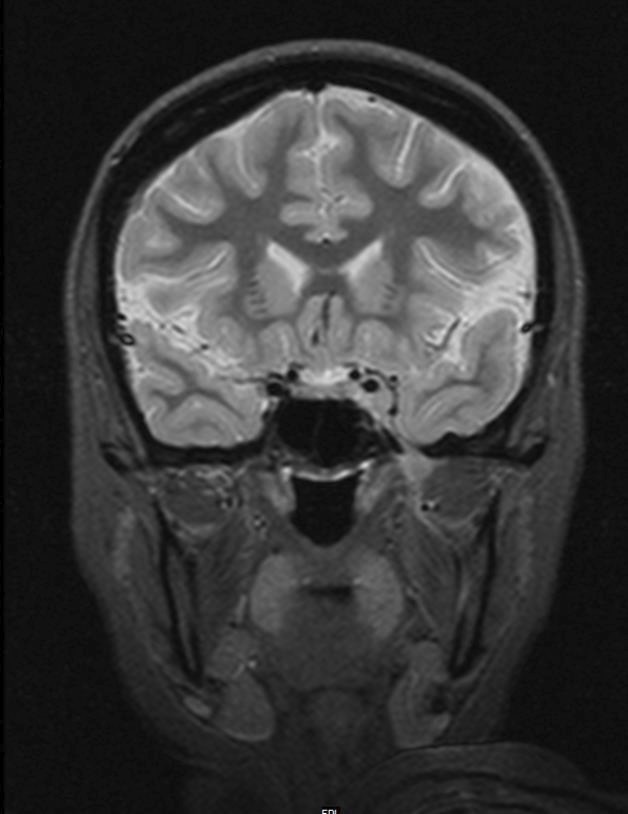

Figure 2: Magnetic resonance imaging (MRI) of the head and orbit axial cut (2a) and coronal cut (2b) showing an avidly enhancing mass in the left cavernous sinus measuring 22mm x 7mm͘. The massextended to orbital apex but there was no intra-orbital extension͘. The left optic nerve was not compressed͘. Imaging appearances raised suspicion of lymphoma or inflammatory aetiologies͘.
Diagnosis and management
Patent was treated as Tolosa-Hunt Syndrome and she responded well with intravenous methylprednisolone with a four-month tapering course of oral prednisolone, she responded very well to steroid treatment, the patent was referred to the medical team to commence zathioprine as steroid-sparing immunosuppression. However, this had to be withheld as a screening interferon-gamma released assay (IGR) T-spot TB test showed positive results. The infectious diseases team was consulted, who started the patent on three-month ant-tuberculosis therapy regimen of Pyridoxine and Rifampicin for latent TB prior to starting zathioprine. CT thorax, abdomen and pelvis further demonstrated multiple calcified granulomata consistent with previous TB exposure (Figure 3)͘. There were no significantly enlarged lymph nodes amenable to biopsy.
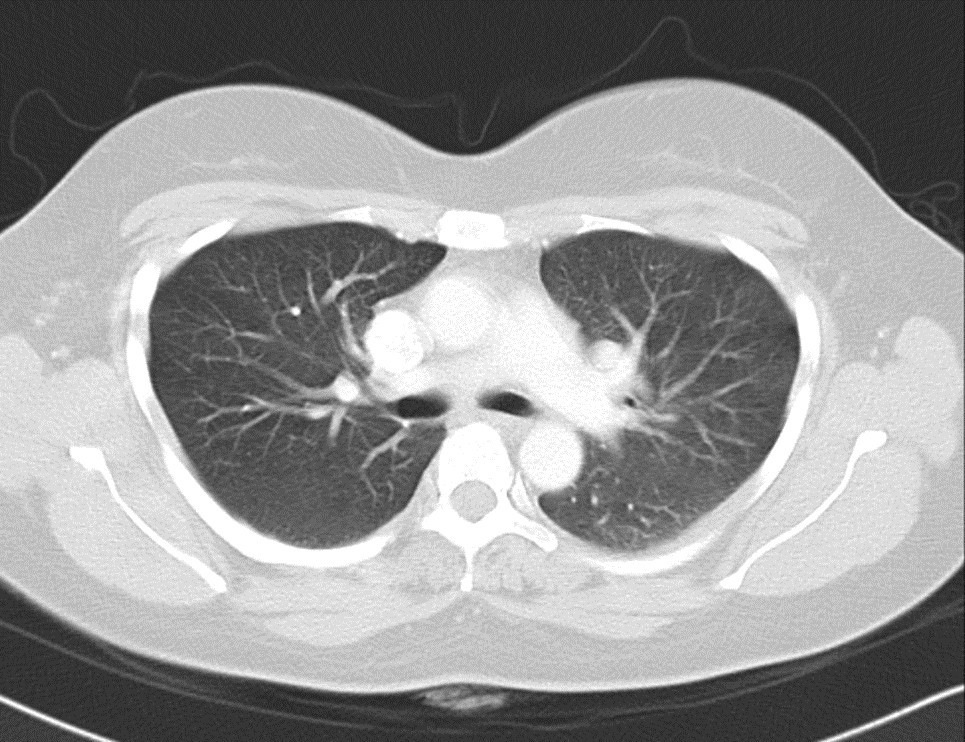
Figure 3: Computerised tomography of Thorax showing multple calcified granulomata consistent with previous Tuberculosis (TB) exposure. No other visceral involvement of TB was demonstrated.
Follow-up
She was followed up every 6 months in the eye clinic with stable clinical and radiological findings and was subsequently discharged. She had received azathioprine treatment for four years and as the follow-up MRI showed no residual actve disease, zathioprine was discontnued. She remained well from an ophthalmological perspectve since.
Discussions and Conclusions
Tolosa-Hunt syndrome (THS) is a rare disease with an estimated incidence of 1-2 cases per million populaton1, characterised by orbital, periorbital or hemi cranial pain with either partial or complete ophthalmoplegia or ptosis, caused by granulomatous inflammation of the cavernous sinus and/or superior orbital fissure which may lead to the compression of any structures contained within2.
According to the 3rd International Classification of Headache Disease (ICHD-3), to diagnose THS, a patent must have granulomatous inflammation of the cavernous sinus, superior orbital fissure or orbit demonstrated by MRI or biopsy, in addition to paresis of one or more of the ipsilateral third, fourth and/or sixth cranial nerves3. In this case, the patent had initial presentation which only fulfilled part of the THS ICHD-3 criteria given the normal imaging findings. The diagnosis of THS was only confirmed when she presented five years later with a left cavernous sinus lesion which responded very well to corticosteroid treatment. Subsequent positive T-spot TB test performed prior to commencing immunosuppression confirmed an underlying latent TB infection, which in retrospect, should be ruled out prior to commencing steroid treatment and before considering THS as a diagnosis͘. Untreated TB might be exacerbated by steroid treatment and immunosuppression could lead to reactivation of TB if not managed carefully.
This case depicts interesting diagnostic and management challenges. Diagnosing THS requires careful evaluation of other possible causes so that any other infective aetiologies are not missed, case series demonstrated a 40% false negative rate and a 40% false positive rate of diagnosing THS4. 18-33% of patents with THS also initially had normal imaging findings5. The initial CT and MRI imaging of our patent did not show obvious cavernous sinus abnormalities and the diagnosis of latent TB was not identified until much later when immunosuppression was already commenced. Cortcosteroid remains the definitive management of THS and steroid sparing agents such as zathioprine can help to reduce recurrence from around 50% to 20%͘6. Yet, there is no definitive steroid regimen in terms of dose or duration of treatment. Generally, a course of high-dose steroids (>05-1mg/kg) is prescribed with a slow tapering over 3-4 months2.
Immunosuppressants are used in the treatment of THS, in areas with high prevalence of TB, it is important to screen for latent infection prior to initiation of treatment. Although we screened this patent initially for TB using Mantoux test, this appeared to be inadequate when the T-spot test performed following her second presentation showed positive results. IGR T-spot tests which have a higher sensitivity and specificity than tuberculin-skin testing7 should be used to improve diagnostic accuracy and confidence of excluding TB as a potential cause prior to establishing the diagnosis of THS.
In conclusion, THS in the context of a patent with latent TB could pose diagnostic and management dilemma. THS is a diagnosis of exclusion which requires extensive investigation into other causes of ophthalmoplegia prior to arriving to that diagnosis. Tuberculoma in the cavernous sinus presenting as cavernous sinus syndrome is a possible cause for the presentation and has been reported in the literature8, but biopsy of the cavernous sinus lesion itself is technically difficult and invasive. Clinicians should therefore rely on less invasive investigations which are more effective at detecting TB infection and cavernous sinus lesions, such as IGR and Gadolinum-enhanced MRI respectively prior to establishing the diagnosis of THS. Latent infection such as TB should be completely ruled out prior to commencing corticosteroid or immunosuppressive treatment for THS.
References
- Iaconeta G, Stella L, Esposito M, Cappabianca P Tolosa-Hunt syndrome extending in the cerebello-pontne angle Cephalalgia 2005;25(9):746-750
- Gladstone JP n approach to the patent with painful ophthalmoplegia, with a focus on Tolosa-Hunt syndrome Curr Pain Headache Rep 2007;11(4):317-325
- Zhang X, Zhou Z, Steiner TJ, Zhang W, Liu R, Dong Z, Wang X, Wang R, Yu S Validaton of ICHD-3 beta diagnostc criteria for 137 TolosaHunt syndrome: analysis of 77 cases of painful ophthalmoplegia Cephalalgia 2014;34(8):624-632
- Mullen E, Rutland JW, Green MW, Bederson J, Shrivastava R Reappraising the Tolosa-Hunt Syndrome Diagnostc Criteria: Case Series Headache 2020 Jan;60(1):259-264 doi:101111/head13692 Epub 2019 Nov 4 PMID: 31681980
- Manta LL, Curone M, Rapoport M, Bussone G Tolosa-Hunt syndrome: critcal literature review based on IHS 2004 criteria Cephalalgia 2006; 26: 772-781
- rthur, Sivadasan, Mannam P, Prabakhar T, aron S, Mathew V, et al͘ Tolosa-Hunt Syndrome: Long-Term Outcome and Role of Steroid-Sparing gents nn Indian cad Neurol͘ 2020 Mar-pr;23(2):201-205
- Oh CE, Ortz-Brizuela E, Bastos ML, Menzies D Comparing the Diagnostc Performance of QuantFERON-TB Gold Plus to Other Tests of Latent Tuberculosis Infecton:Systematc Review and Meta-analysis͘ Clin Infect Dis͘ 2021;73(5):e1116-e1125 doi:101093/cid/ciaa1822
- Kodera T, Takeuchi H, rishima H, Tsunetoshi K, Kitai R, rai Y, Kikuta KI, Hamano T, KuronumaY Microsurgical findings of Tolosa-Hunt syndrome World Neurosurgery 2013 Mar 1;79(3-4):594-e1
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds