Post-op cystoid macula odema
Patient presentation
I had referred an 80 year old patient for left cataract surgery in September 2023. She had previously had uncomplicated right cataract surgery. She does not have a history of any other ocular surgery or conditions.
She has rheumatoid arthritis, for which she is taking medication, but is otherwise in good health. She attends hydroxychlroquine screening at the local hospital eye service and reports that the results have always been clear.
This patient presented for a post-cataract op assessment in December 2023 for her left eye. She reported that she felt her vision had not improved as much as it had after having her right eye cataract surgery. She has mild amblyopia in her left eye, and she felt this could be why she had not noticed an improvement.
BCVA was 6/15 in the left eye after cataract surgery (no improvement from pre-op VA).
She also reported during the sight test that when I occluded her right eye, the line of letters on the Snellen chart would appear distorted. This led me to believe there may be some post-op CMO and thus I carried out an OCT examination.
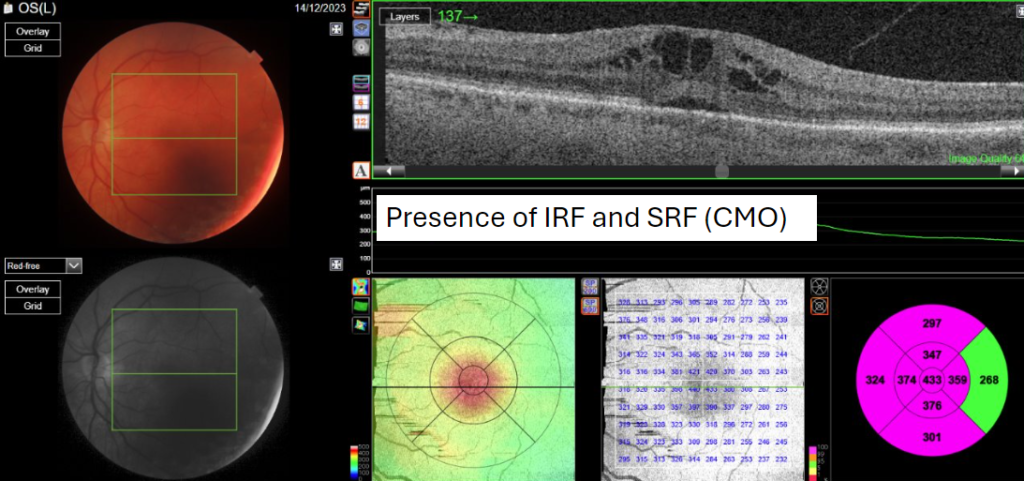
OCT confirmed my suspicions as post-op cystoid macula odema as well as an epiretinal membrane.
Diagnosis and Management
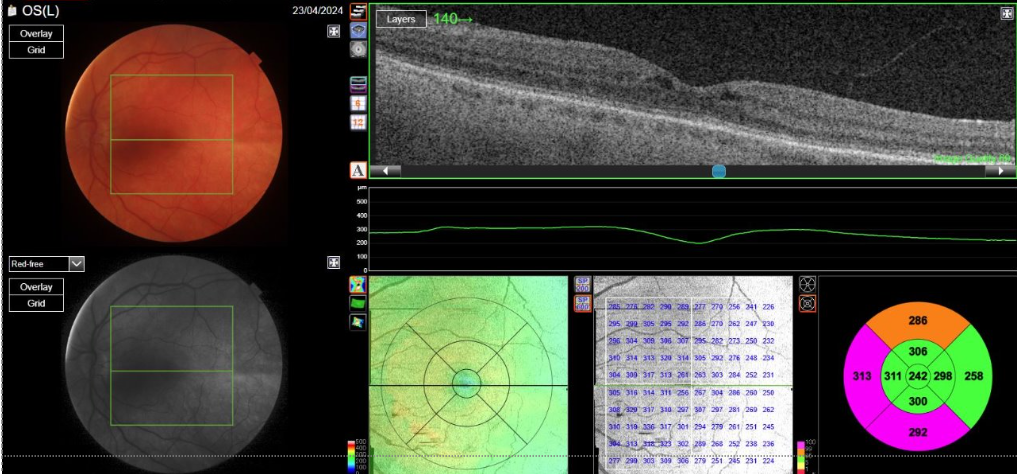
The patient was referred back to the operating hospital for this. She was prescribed a course of Prednisolone and Acular, and reviewed 4 weeks later. At the 4 week review, there was still CMO present and so she was advised to continue with the medication for another 8 weeks. She was reviewed 8 weeks later and was told that the CMO had improved, but she would still need to continue with the medication and be monitored at the hospital. At this point, the patient chose to self-discharge and stopped using the drops shortly after, as she ran out of them.
The patient returned a month after discharge. Her main complaint was that she was struggling with reading, as she had not had an up-to-date pair of reading glasses since before her cataract surgeries.
She told me she had chosen to self-discharge because she found it difficult to attend the hospital as she had poor mobility and relied on transport from family and friends. She felt she had been a burden to those around her because she had to keep going back to the hospital for follow-up appointments due to the persistent CMO.
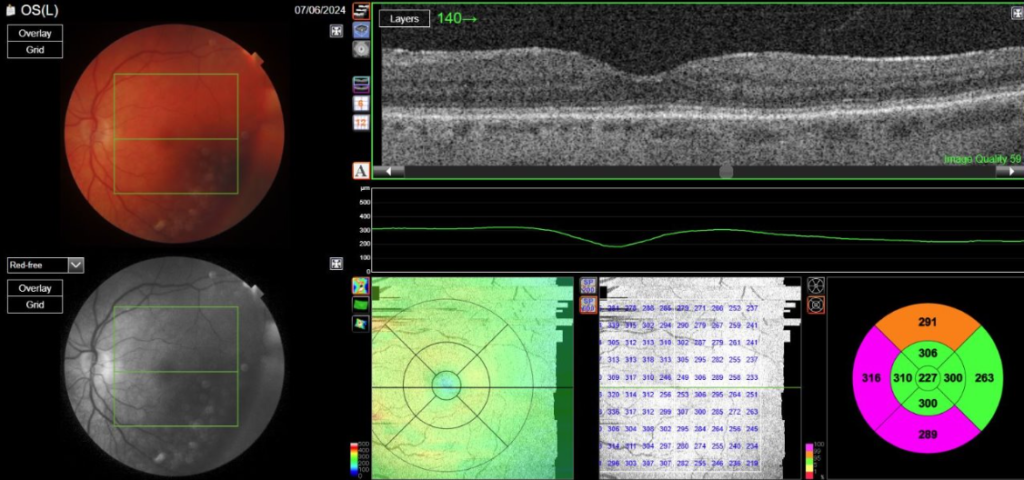
In the case of this patient, when she returned for her check-up with me after discharge, OCT showed a relapse in the CMO.
Conclusion
This patient had difficulty accessing the hospital because she was elderly, a non-driver, and had mobility difficulties. This caused her unnecessary stress, as she felt she was being a burden to the people around her. She lives alone and is usually independent, so this was something she found distressing. If I had been able to prescribe the medication and monitor her in the community, it would have been much easier for her as she lived within walking distance from the practice. It is likely the relapse in CMO could have been avoided.
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds