Diagnosing and Treating Inflammatory OSD(Ocular Surface Disease)

Clinicians are much more aware of this disorder due to the large amount of research published in the past few years, e.g. Delphi Panel Treatment Guidelines (2006), the International Dry Eye Workshop (DEWS) (2007) and the Meibomian Gland Dysfunction (MGD) Workshop (2011). With this research, diagnosis and treatment can be tailored to the specific disease subtype as well as the severity of the condition.
Several factors have made OSD challenging to manage – complex aetiology, poorly understood pathophysiology, overlap of different OSD subtypes, poor correlation between clinical symptoms and signs, lack of diagnostic technology and limited treatments.
OSD in most patients tends not to manifest as a red eye, but inflammation is still present. It can cause high morbidity and significant ocular surface damage.
There are many risk factors and multiple risks factors may be present. Occasionally, determining exact aetiology is not possible or there may be multiple aetiological factors contributing to OSD but treatment is important.
Aetiological factors include age, female/male, medications, environmental and occupational factors e.g. screen time, local conditions such as rosacea, sarcoid, allergy and contact lens wear; systemic conditions e.g. rheumatoid arthritis, lupus, diabetes mellitus, Sjogren’s, chemotherapy and mucous membrane pemphigoid.
Symptoms and signs may not correlate which makes diagnosing challenging. This is probably due to different microbiome on the ocular surface, varying sensory innervation (reduced or increased) of the ocular surface and varying levels of inflammatory markers.
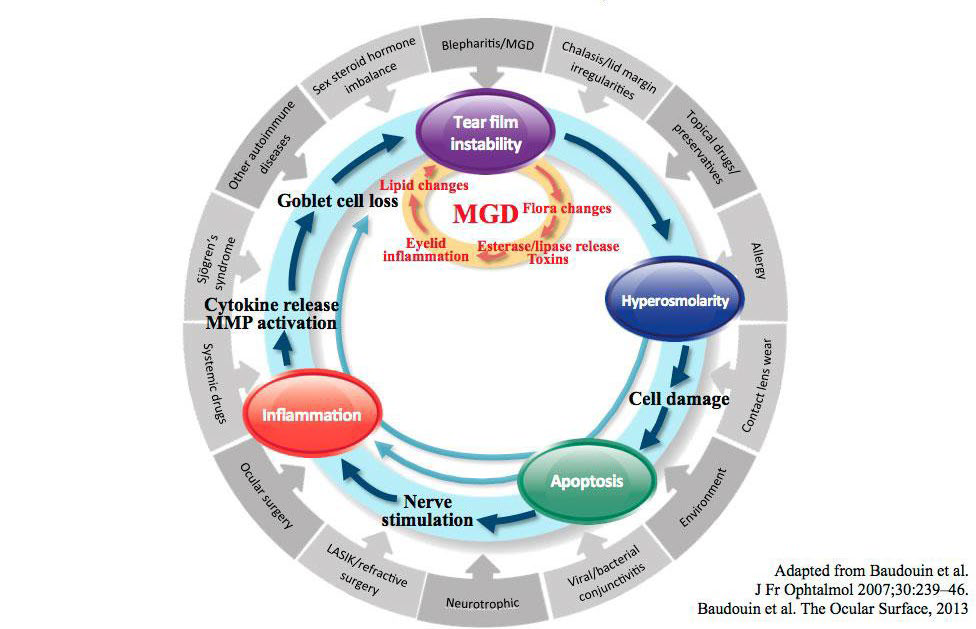
Key Mechanisms of Dry Eye Disease: The Vicious Circle Theory
Inflammation is an important concept to identify in OSD. Once there is a significant level of inflammation on the ocular surface, the patient will need anti-inflammatory treatment to break this vicious cycle of inflammation in order to improve symptoms. Most patients obtain great relief once the inflammation is under control. A subset of patients may have recurrent inflammation so more prolonged anti-inflammatory treatment is required.
Diagnosing OSD
In most clinical settings, an OSD/dry eye questionnaire (e.g. ODSI), a thorough medical history and a slit-lamp examination (TBUT and corneal staining) are sufficient in diagnosing OSD.
However, if a patient doesn’t improve with initial treatment (e.g. lid hygiene, topical lubrication, adjusting environmental factors), then a referral to an OSD clinic is recommended.
OSD Clinic
Step 1
In an OSD clinic, the patient completes a medical history form requesting information on medical history, ocular history including surgical history and contact lens use, medications (ocular and systemic), allergies, current symptoms and previous treatments for OSD. They also complete an OSDI questionnaire which will aid in the grading of the severity of their symptoms.
Step 2
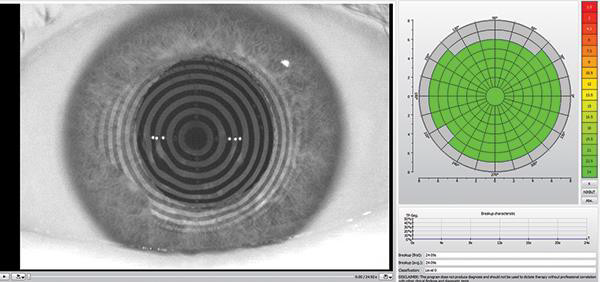
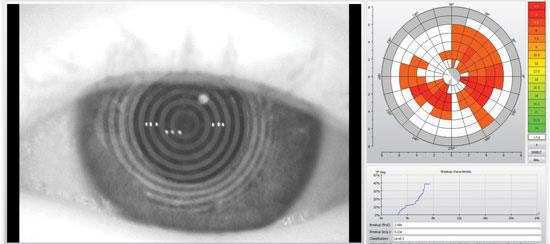
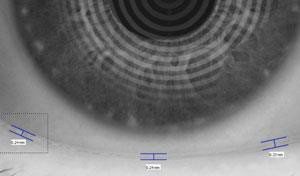
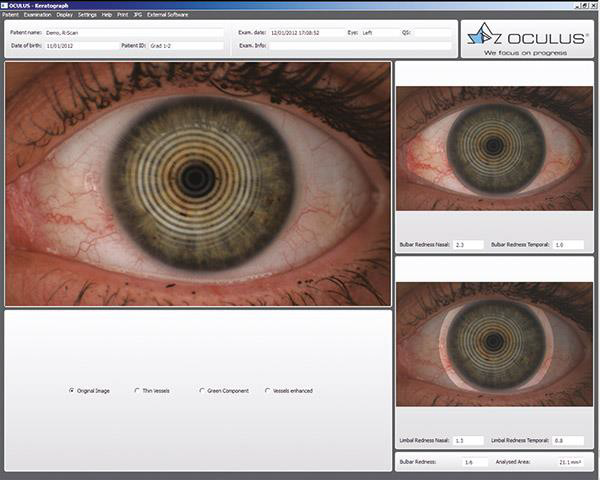
An Oculus Keratograph 5M is performed which gives valuable clinical information. It is an advanced corneal topographer with dry eye software which examines:
- Tear meniscus height (TMH)
- Non-invasive tear break-up time (NIBUT) which measures the TBUT without a fluorescein drop therefore making it highly accurate
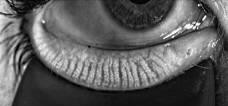
- Meibomian glands using meibo-scanned images. Meibomography findings may be more significant than clinical signs of MGD
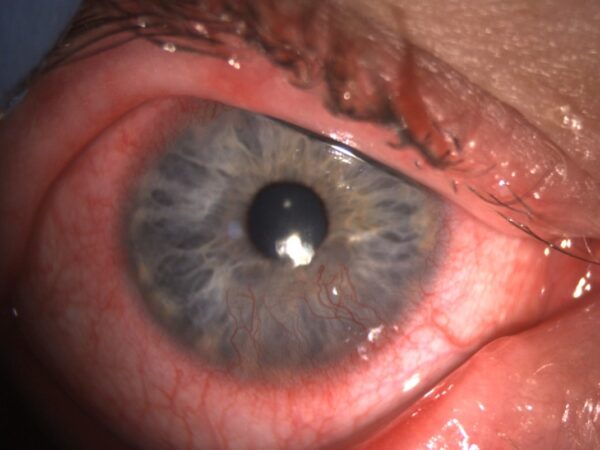
- The degree of ocular inflammation using R-scans
- Lipid layer analysis
- Additional diagnostic tests include osmolarity of the tears and inflammatory markers e.g. MMP-9 (variable results).
- Schirmer’s test measures the patients tear volume.

Step 3
Visual Acuity
Slit lamp examination includes thorough examination of lids/conjunctiva and meibomian glands. Expression of the meibomian glands is important to assess the meibum. Assess the lid margin and lashes. Lid closure, malposition of the lid and partial/incomplete blinking are important signs to assess. Evert the lids to assess the tarsal conjunctiva. Evaluate corneal sensation (normal, decreased or none) with a cotton bud tip.
The cornea can be examined with fluorescein and lissamine green staining. In some OSD cases, conjunctival staining may be present rather than corneal staining e.g. in ocular rosacea, so it is important to use lissamine green.
With all this information, a diagnosis is made and a treatment plan started.
Types of Dry Eye Disease
There are two main subtypes of OSD/DED:
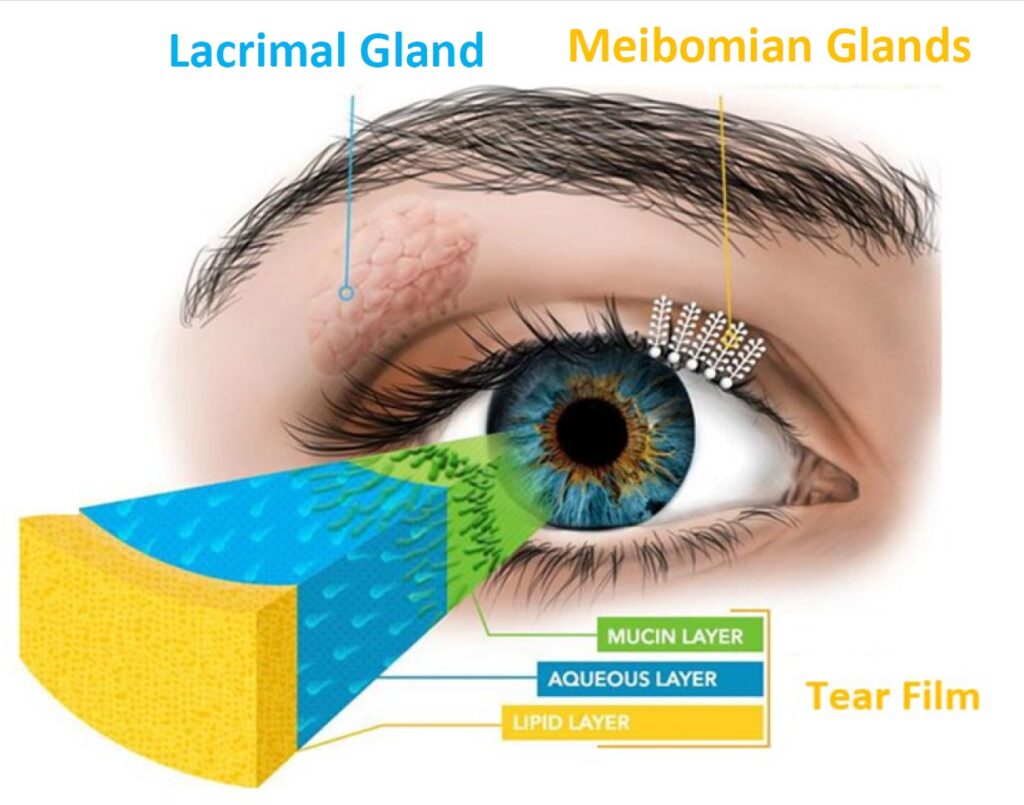
- Evaporative Dry Eye which is mainly caused by MGD.
- Aqueous Deficient Dry Eye is characterised by a reduction in the secretions from the lacrimal gland (main and accessory glands) that form the aqueous component of the tear film.
Two other subtypes are identifiable in some cases…
- Goblet cell deficiency/mucin deficiency e.g. Steven-Johnson Syndrome, pemphigoid, thermal and chemical injuries, contact lens wear and epidemic keratoconjunctivitis (EKC).
- Exposure-related OSD (lid dysfunction/malposition, poor or partial blink e.g. bells palsy and lagophthalmos). The presence of multiple subtypes is common.
The majority of the cases seen are the evaporative type (85%), mostly due to MGD.
Aqueous deficient DED tends to show more severe clinical signs. Serological testing can help if there is a high index of suspicion for systemic conditions e.g. Sjogren’s Syndrome, SLE, rheumatoid arthritis etc.
It is important to try and diagnose the subtype as treatment plans differ. However, there may be an overlap/mix of diagnoses.
OSD co-conspirators are conditions affecting the ocular surface/tear film that may masquerade or exacerbate OSD. They include ocular allergy (a common co-conspirator), SLK, medication, contact- lens-related toxicity, mucus fishing syndrome, conjunctivochalasis, floppy eyelid syndrome and Thygeson’s superficial punctate keratitis. It is important to identify and treat conditions to improve patient’s symptoms.
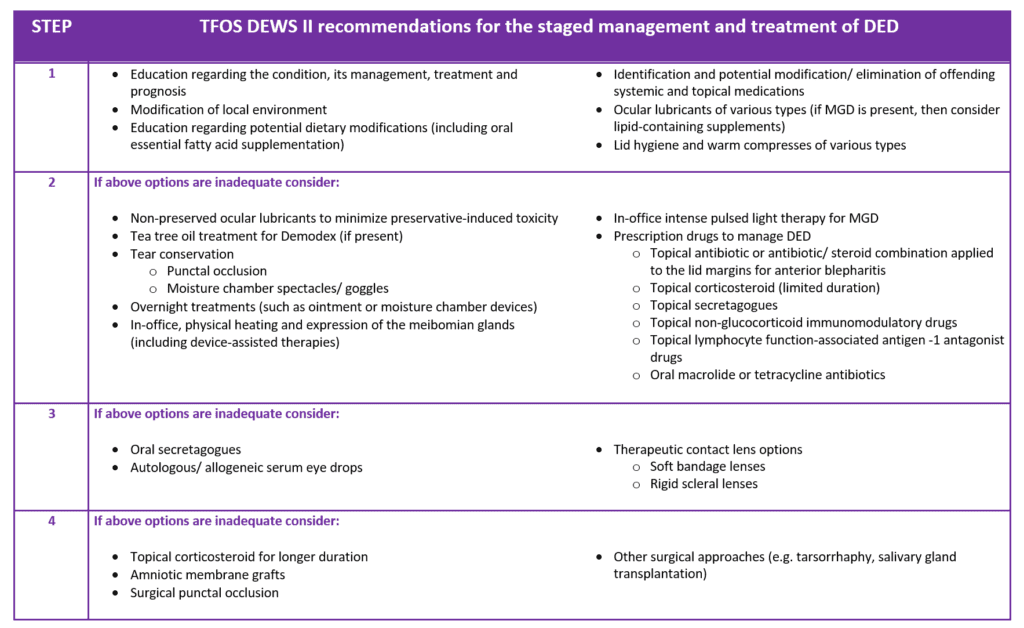
Treatment and Management of Dry Eye Disease
Full explanation and counselling are important when treating the patient. When the patient is empowered with information, compliance with treatment is higher. This is vital as OSD is a chronic condition which requires on-going management.
Treatment is based on symptom and sign severity and a diagnosis-based individualized treatment approach is taken.
Lid hygiene and regular topical lubrication is a base-line treatment and tends to be sufficient for mild OSD/DED.
Tea-tree oil wipes play a role in reducing lid inflammation and Demodex. Regular topical lubrication is important even when inflammation is under control. If more severe, anti-inflammatory treatment is started. This breaks the vicious inflammatory cycle of OSD.
Topical steroids such as “soft” topical steroids (i.e. have poor penetration of ocular surface and less steroid side effects such as raised IOP and cataract) are used. Other anti-inflammatory treatments include topical cyclosporine or topical tacrolimus may need to be used. Future immunomodulatory and target specific topical drugs will be available in the near future e.g. Lifitigrast which is available in the US, ACE drops (Amniotic cytokine extract) and Recombinant DNase eye drops. Occasionally, systemic immunosuppression may be required.
Systemic disease needs to be controlled in order to improve OSD e.g. Rheumatoid arthritis, SLE, rosacea so referral to a physician may be appropriate.
A novel nasal spray (contains a nicotinic acetylcholine receptor agonist to stimulate the trigeminal parasympathetic pathway to increase tear production) is showing promising results.
Intranasal tear neurostimulation involves an external, non-implantable device to stimulate the nasal mucosa and activate the nasolacrimal reflex to increase tear production and improve tear film homeostasis.
Punctal plugs are used early on in aqueous deficient DED. They play a role in evaporative DED but it is initially treated medically (i.e. drops, topical or oral antibiotics) as insertion of punctal plugs early may lead to the accumulation of “toxic” tears which worsens symptoms.
Rarely, surgical treatment (see table below) is required:
Treatment for MGD
Systems which improve expression of meibomian glands include:
- External heat including a hot compress, automated eye mask.
- Internal heat (more efficient than external heat) such as Lipoflow (varying results) IPL (varying results) and Thermaeye Plus Eye-Light.
- BlephEx, a rotatory brush made specifically for the lids that cleans the lashes and removes the biofilm/hyperkeratosis from the surface of the meibomian glands.
There are a large number of products on the market but further studies do need to be carried out in order to improve success rates.
A basic OSD checklist includes:
- Identify ocular surface problems
- Patient involvement
- Address local factors
- Address systemic factors
- Nutrition and hydration
- Modify environment
There is a high incidence of chronic pain syndrome amongst OSD/DED patients. It has been highlighted on QOL (quality of life) index. There is a high level of disability and mental health issues with a subgroup of patients. This can be treated with pain management techniques and with a pain management team, thus improving the patients’ overall wellness.
Patient education and counselling is vital so that the patient understands and complies with treatment plans and feels in control of this chronic condition resulting in better outcomes.
Improving the ocular surface is also important to reduce distressing symptoms and improve visual acuity and quality of life in inflammatory OSD. It is also crucial for pre-cataract and refractive surgery patients as it can have a negative impact on surgical outcomes. Important measurements e.g. biometry, keratography may not be accurate if OSD is not treated. Also, OSD/DED can be worse postop (acute flare-up) if not tackled preop resulting in poor visual outcomes and unhappy patients.
While treating OSD/DED can be complex, our understanding of the condition has greatly increased the past few years and diagnosis and treatments have greatly expanded with improved patient outcomes and increased patient satisfaction.
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds