A Rare Case of Bilateral Periocular Swelling
Patient Presentation & Diagnostic Testing
A 38-year-old woman presented to her general practitioner with bilateral slow progressive peri-ocular swelling and was referred to the haematologist two years ago. The referral was initiated due to the patient’s recent suspected diagnosis of lymphoma prior to relocating from Ghana to the UK.
The patient underwent a bone marrow biopsy in Ghana, which indicated a resemblance to lymphoma and had plans to initiate chemotherapy. However, due to relocation to the UK, the chemotherapy was not pursued.
Concurrently, the patient reported experiencing asthma-like symptoms persisting for the past 8 months an was started on inhaler therapy. Notably, there were no significant past medical history findings apart from this. The systemic review revealed apyrexia, no weight loss, occasional vomiting, severe headaches, and absence of night sweats. The patient had a non smoking history, consumed alcohol occasionally, was currently unemployed, and was married with two children. Blood tests were ordered by the haematologist to establish a baseline and look for any possible infective, inflammatory, and malignant causes, these tests included FBC, U&E’s, TFTs ESR, Ca, LDH, para protein and viral serology – all values were within the normal range.

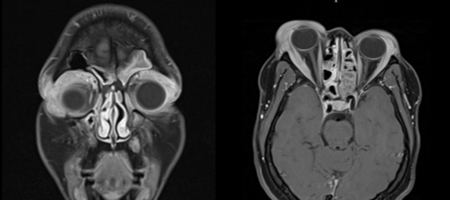
On orbital CT, there was evidence of presentation of orbital masses. Furthermore, there was also axillary lymphadenopathy but no lymphadenopathy anywhere else. The possible differential diagnosis for axillary lymphadenopathy are; infections (such as tuberculosis, HIV etc.), inflammatory (lupus, rheumatoid arthritis) or malignant causes (lymphomas or other carcinomas).
The MRI scan revealed a normal intracranial appearance with potential sinonasal polyposis accompanied by secondary sinusitis. Furthermore, there was a significant enlargement observed in both lacrimal glands, with the right gland exhibiting a greater increase in size. The enlargement extended into the upper eyelid and posteriorly along the lacrimal walls. The findings, thus far, were more in keeping with a diagnosis of lymphoma but, a biopsy was needed to confirm.
By now, the patient had started to experience worsening eye swelling, diplopia, headaches, and vomiting – this was suspected to be a disease of a progressive nature.
A bone marrow biopsy eliminated lymphoma, however, the eyelid biopsy of the periorbital lesions showed ‘foamy macrophages’, the presence of this indicated a possible inflammatory cause, thereby making lymphoma a less likely diagnosis. Due to this histological diagnosis, Langerhans cell histiocytosis was considered as a possible differential. Langerhans cell histiocytosis is the collection of rapidly dividing Langerhans cells in various areas across the body, its often encountered more in paediatric patients however, adults are known to have been diagnosed as well.
Due to the emerging picture of an inflammatory, as opposed to a neoplastic cause, the patient was provisionally started a tapering dose of prednisolone (starting at 60mg, being reducing by 10mg on a weekly basis) and lansoprazole.
However, after stating the course of prednisolone, the patient gradually began to develop steroid-induced diabetes and gastritis, this prevented any further use of them.
Due to the complexity of this case the patient was referred to the National Langerhans Cell Histiocytosis Multi-disciplinary Team (MDT). This meeting, provides specialist opinion on the management of disorders of a histiocytic nature, they subsequently advised to commence the patient on an immunosuppressive agent, Methotrexate 20mg OD, for three months (as it could take up to 3 months to see an effect).
Weeks after commencing oral Methotrexate and weaning off the oral prednisolone, the patient presented to ED unwell, with worsening significant right eye swelling, feeling weak, vomiting, photophobic. This prompted the use of 10mg prednisolone with talks of further discussion with the national MDT.
A CT of the chest, abdomen and pelvis was conducted ahead of the MDT which showed stable appearances if the prominent left axillary lymph node and no new significant abnormalities. However, the MRI showed some reduction of disease in the orbits but, still persistent. By now, the patient had been on methotrexate for 11 months and showed only mild response.
The National Langerhans Cell Histiocytosis MDT advised the following recommendations for the management of this complex case: (1) consideration of initiating a new agent, such as Rituximab, supported by available evidence in the literature, (2) obtaining an ophthalmology opinion to assess the feasibility of debulking the lesions, (3) exploration of alternative agents, including cyclophosphamide, sirolimus, imatinib, and thalidomide, despite their limited utilization thus far, as they hold potential therapeutic value. The final decision regarding the management approach was contingent upon the patient’s preferences and treatment objectives.
The patient expressed hesitancy regarding the initiation of Rituximab or any other immunosuppressive agents, primarily due to the poor response observed thus far with methotrexate in reducing the periocular swelling. Additionally, concerns were raised regarding the potential impact of these medications on her desire to have children in the near future. Moreover, the patient was also not keen on further immunosuppression as she was considering her fertility. The patient therefore opted to be assessed for possible surgical debulking and was therefore referred to ophthalmology A referral was made to have the patient seen in the ophthalmology specialist orbital clinic.
Presentation at the oculoplastic orbital clinic & Diagnosis
The findings previously present of significant bilateral orbital swelling along the upper orbital areas remained with the additional appearance of right ocular proptosis. The periorbital masses were firm to palpation, more prominent on the right than the left side. Eye movements were reasonable with no signs of limitation. Intraocular examination was normal, and optic nerve function test were unremarkable with a healthy appearance to the optic nerves on fundoscopy.
Due to the complexity of the condition, the patient was referred to Moorfields Eye Hospital for an orbital biopsy. The results showed the tissue to consist of reactive lymphoid follicles (histiocytic lesion).
The patient was subsequently diagnosed with Adult-onset Asthma with Periocular Xanthogranuloma (AAPOX), this is part of a rare category of diseases that is known to affect the orbital and periorbital tissue by the deposition of infiltrative material in these areas [1,2].
Management
Thus far, the patient showed an improved response with an increased dose of prednisolone however, as mentioned previously, the development of steroid-induced diabetes and gastritis, limited the use of higher doses of prednisolone.
The patient preferred a non-surgical route, this prompted us to try intralesional Triamcinolone steroid injection before attempting more invasive options such as surgical debulking.

Previous cases, in the literature, have received up to 120mg of Triamcinolone in one setting, with up to 40mg to each site of nodularity and repeated injections had been given at once every 6 months in the past [6]. Based on these cases, we injected 40mg to each upper eyelid, as demonstrated in figure 3. After the first round of injections, lesions were a lot less firm, and patient perceived a benefit from them so preferred to continue with round 2 and 3. Injections repeated 4-6 weekly intervals up to six times in a course. The only complication experienced was mild intralesional bleeding in the period directly following the injection.
Follow-up & Discussion
Adult orbital xanthogranulomatous disease (AOXGDs) are a group of relatively rare diseases that are known to affect the orbital and periorbital tissue by the deposition of infiltrative material in these areas. There are currently four entities that form part of this disease, each appearing histopathologically distinct: necrobiotic xanthogranuloma (NBX), Adult onset xanthogranuloma (AOX), adult-onset asthma and periocular xanthogranuloma (AAPOX), and Erdheim-Chester disease (ECD). AAPOX lies on a spectrum of IgG4-related disease [1,2].
Owing to the rare nature of the condition, there is little known about the effectiveness of therapeutic modalities to treat them [1,2]. Current treatment strategies include the use of systemic steroids [3,4], antimetabolite agents such as methotrexate [4,5], debulking surgery [5,3], and intralesional corticosteroids [6].
As mentioned earlier, the evidence-based treatment of this condition is limited due to its rarity. Some studies have employed the use of systemic steroids, these are often cheap and readily available however, the clinical response seen is often only partial, with several authors reporting the recurrence of symptoms on tapering the medication. Alongside this, the use of this therapy is associated with the usual side-effect profile seen with the use of systemic steroids [3,4]. In the case of our patient, the use of oral prednisolone led to the onset of steroid-induced diabetes and gastritis which limited the use of doses higher than 10mg of prednisolone.
Other studies used antimetabolite agents such as maintenance low-dose methotrexate and azathioprine, these have been used to successfully achieve disease remission in AAPOX, however, there is seemingly a significant side effect profile, such as gastrointestinal issues and fatiguability, associated with systemic use that can potentially make compliance an issue [4,5,7]. In our patient, the bilateral periorbital swellings respond only mildly to methotrexate due to which it was discontinued.
The application of local radiotherapy as a treatment modality in AAPOX has been thus far limited, its use has been trialled as a possible treatment choice with use in variants of AAPOX, such as necrobiotic xanthogranuloma (NBX), however, the results thus far have been mixed with its used being reserved in patients with limited response to steroid treatment as it has been linked to exacerbation of the periorbital lesions [1,8-10].
Surgical debulking has been used in certain cases after a trial of local and systemic therapies, some cases report a positive outcome with no recurrence [1,5] however there is a larger cohort of reports demonstrating the recurrence of the lesions, with the average of 6- 12 months since the surgical procedure [11, 12]. Due to the above reasons and risks associated with surgery, surgical debulking has been left as the treatment of last resort for our patient once all treatment avenues have been exhausted.
Intralesional corticosteroid injections have been used to treat various periocular disease such as thyroid ophthalmopathy [13], however, its used in AAPOX has yielded mixed results [6, 14]. Local use reduces the likelihood of systemic side effects, however, there have been reported cases of adrenal suppression [15]. Alongside this, administration may cause local side effects such as Central Retinal Artery Occlusion (CRAO) [16] and eyelid necrosis [17].

As seen in figure 5, our patient showed an improved response with an increased dose of prednisolone however the development of steroid-induced diabetes and gastritis, limited the use of higher doses of prednisolone. This prompted us to try intralesional steroid injection before attempting more invasive options such as surgical debulking. As demonstrated in the images, our patient responded well initially, however her response plateaued after the third cycle.
A recent study [18] highlighted the role of biologics such as rituximab that, when used in combination with intralesional steroids, have achieve an effective reduction of periorbital lesions in AAPOX, and should be considered as a possible next step in management due to preference for nonsurgical routes by our patient. In the most recent visit to the oculoplastic orbital clinic, the lesion on the left side looked better than previously. The decision was made to refer the patient for orbital debulking and consideration of other aforementioned biologics, as suggested by the MDT in Oxford.
References
- Sivak-Callcott JA, Rootman J, Rasmussen SL, Nugent RA, White VA, Paridaens D, Currie Z, Rose G, Clark B, McNab AA, Buffam Adult xanthogranulomatous disease of the orbit and ocular adnexa: new immunohistochemical findings and clinical review. British Journal of ophthalmology. 2006 May 1;90(5):602-8.
- Guo J, Wang Adult orbital xanthogranulomatous disease: review of the literature. Archives of pathology & laboratory medicine. 2009 Dec;133(12):1994-7.
- Green MB, Daly MK, Laver NM, Lefebvre Adult-onset asthma and periocular xanthogranuloma–A rare infiltrative disease of the orbit and eyelid. American Journal of Ophthalmology Case Reports. 2021 Jun 1;22:101043.
- Hayden A, Wilson DJ, Rosenbaum Management of orbital xanthogranuloma with methotrexate. British journal of ophthalmology. 2007 Apr 1;91(4):434-6.
- Kusumgar P, Vijaya PH, Monappa Adult-onset asthma and periocular xanthogranuloma: A rare case report. Canadian Journal of Ophthalmology. 2016 Dec 1;51(6):e168-71.
- Elner VM, Mintz R, Demirci H, Hassan Local corticosteroid treatment of eyelid and orbital xanthogranuloma. Transactions of the American Ophthalmological Society. 2005 Dec;103:69.
- Smith JR, Rosenbaum A role for methotrexate in the management of non-infectious orbital inflammatory disease. British journal of ophthalmology. 2001 Oct 1;85(10):1220-4.
- Burris CK, Rodriguez ME, Raven ML, Burkat CN, Albert Adult-onset asthma and periocular xanthogranulomas associated with systemic IgG4-related disease. American journal of ophthalmology case reports. 2016 Apr 1;1:34-7.
- Kerstetter J, Wang Adult orbital xanthogranulomatous disease: a review with emphasis on etiology, systemic associations, diagnostic tools, and treatment. Dermatologic clinics. 2015 Jul 1;33(3):457-63.
- Ebrahimi KB, Miller NR, Sassani JW, Iliff NT, Green Failure of radiation therapy in orbital xanthogranuloma. Ophthalmic Plastic & Reconstructive Surgery. 2010 Jul 1;26(4):259-64.
- Zoumalan CI, Erb MH, Rao NA, See R, Bernstine MA, Shah SB, McCulley Periorbital xanthogranuloma after blepharoplasty. British journal of ophthalmology. 2007 Aug 1;91(8):1088-9.
- Salvador JO, Ferrer DS, Ferriols Adult xanthogranulomatous disease of the orbit: clinical presentations, evaluation, and management. Actas Dermo-Sifiliográficas (English Edition). 2017 Jun 1;108(5):400-6.
- Bagheri A, Abbaszadeh M, Yazdani Intraorbital steroid injection for active thyroid ophthalmopathy. Journal of ophthalmic & vision research. 2020 Jan;15(1):69.
- Bijlsma WR, van den Bosch WA, van Daele PL, Paridaens Azathioprine and prednisone combination treatment for adult periocular and orbital xanthogranulomatous disease. Acta ophthalmologica. 2011 May;89(3):e278-82.
- Weiss Adrenal suppression after corticosteroid injection of periocular hemangiomas. American journal of ophthalmology. 1989 May 1;107(5):518-22.
- Egbert JE, Schwartz GS, Walsh Diagnosis and treatment of an ophthalmic artery occlusion during an intralesional injection of corticosteroid into an eyelid capillary hemangioma. American journal of ophthalmology. 1996 Jun 1;121(6):638-42.
- Sutula FC, Glover Eyelid necrosis following intralesional corticosteroid injection for capillary hemangioma. Ophthalmic Surgery, Lasers and Imaging Retina. 1987 Feb 1;18(2):103-5.
- Asproudis, , Kanari, M., Ntountas, I., Ragos, V., Goussia, A., Batistatou, A. and Voulgari, P.V., 2020. Successful treatment with rituximab of IgG4-related disease coexisting with adult-onset asthma and periocular xanthogranuloma. Rheumatology International, 40(4), pp.671-677.
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds