Orbito-Zygomatic Ostepblastoma: Unusual Lesion, Unusual Location
Patient presentation:
A healthy 25 year old presented to eye casualty via their optometrist with intermittent headaches, constant right eye pain, worsening proptosis, vertical diplopia and superior globe displacement over 3 months causing significant facial deformity. He had no tinnitus, unusual sinus discharge, earache or other neurological symptoms.
He was fit and healthy with no past medical history and was not on any regular medication. He was a non-smoker who drove and worked full time. He denied any history of trauma or previous surgery. On examination, his unaided VA was 0.2 logmar bilaterally with right eye having 5mm hyperglobus and 5mm of proptosis in comparison to his left eye.
A palpable, hard mass in the right inferior orbit displaced the globe upwards and indented the inferior portion (as shown below). The mass was slightly tender upon palpation and appeared to be adherent to the bone – the under surface was not palpable. There was a change to the zygomatic arch and floor of orbit structure but no nasal deviation. There was no nasal discharge or black eschar. Dilated ocular examination was normal with no increased vascularity, pigmentation, lesions or abnormal intra-ocular pressure. The only abnormality was restricted depression and elevation. He had vertical diplopia in primary position and preferred to wear a patch over this right eye.
Systematically, his basic observations were normal and he reported no weight loss, night sweats or fatigue. There was no history of recent foreign travel or previous facial/ ocular history



Investigations:
An OCT scan showed right choroidal folds with healthy optic nerves suggestive of external globe compression. Vasculature was normal and his left eye was unremarkable.
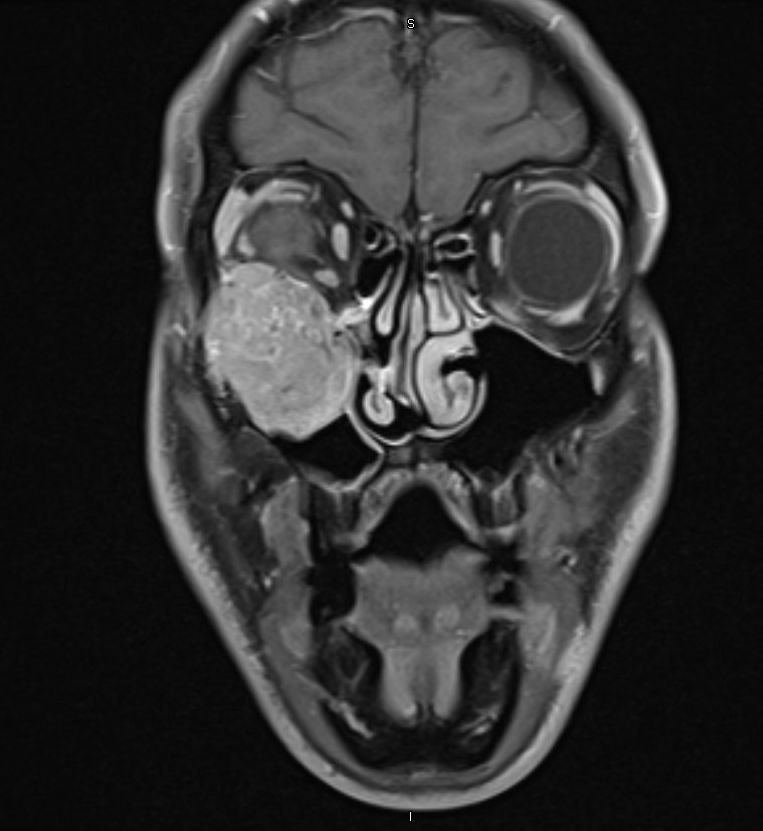
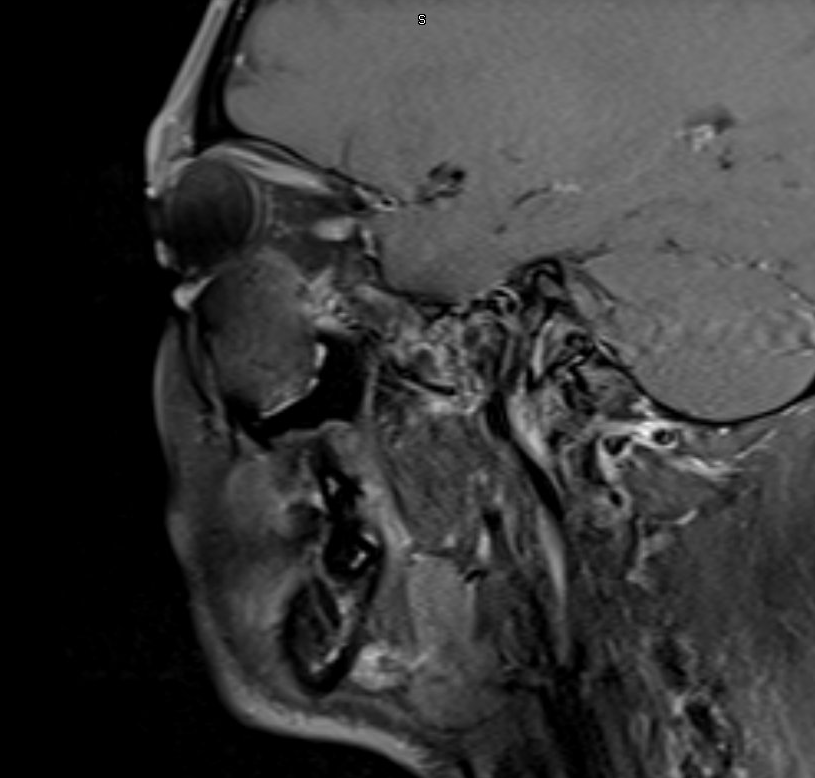
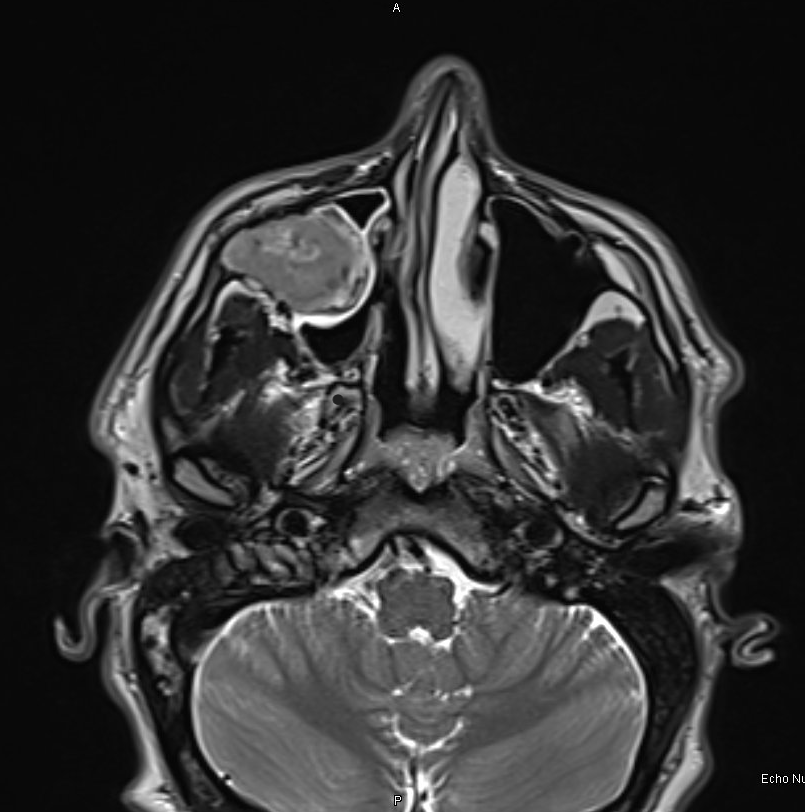
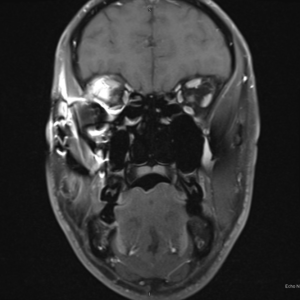
Blood tests (FBC, U&E, CRP, LDH, Calcium, blood film, LFT, ACE, ANA, ANCA, HbA1C, Ig4, LFT, TFT) all returned as normal. Visual fields were full bilaterally. Initial MRI with contrast shows a heterogenous T1/T2 lesion with bony erosion of the orbital floor including the adjacent maxilla and zygomatic arch.
A mass effect on the globe and muscles is evident below. There is no enlargement of the extra-ocular muscles seen or compression of the optic nerve.
Diagnosis and Management:
Differentials:
- Osteosarcoma
- Osteoid tumour
- Lymphoma
- Metastasis
- Neural based tumour
Management:
2 X FESS endoscopic biopsies performed by ENT showed only reactive tissue on pathology and the biopsy was thus considered inconclusive.
The lesion was, however, growing and becoming symptomatically worse. The worry was that the surrounding anatomy would be compromised. This young man’s life had changed and the psychological impact of such a disfigurement was taking its toll.
A MDT decision concluded that a gross total resection should be performed to avoid further anatomical compromise and to obtain a concrete pathology sample.
Thus, an en bloc resection using a Weber-Ferguson incision (shown below) was performed jointly with maxillofacial and the orbital team.

The zygoma arch and lateral maxilla required careful removal to avoid damaging the globe and muscles inferiorly.
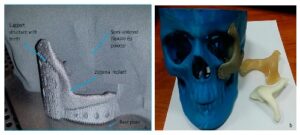
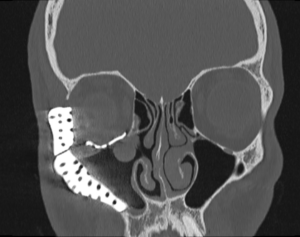
The excised gross lesion was sent to histopathology for diagnosis. Simultaneous reconstruction of the inferior orbit and zygoma wall using a custom-made titanium implant via computer-assisted mirrored coupling technology (similar to shown below) which allowed for a unique post-operative cosmesis.
Histology:
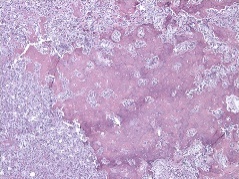
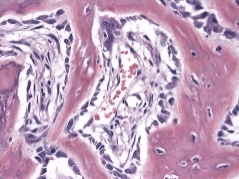
Macroscopically: an excised dark brown maxillary and zygomatic bone lesion measured 54mm x 40mm x 29mm that involved the infraorbital canal was examined.
Microscopically: the tumour composed of anastomosing trabeculae of woven bone rimmed by plump osteoblasts in a vascularised stroma that had broken through cortex but showed no host bone permeation.
No malignancy was identified and the diagnosis of an osteoblastoma was made.
Follow-Up:
Post op Radiological Images:
A 4-month post-op MRI showing the implant with improved globe position and the CT scan demonstrates the titanium implant used to reconstruct the orbital walls that were removed to keep the contour of the facial anatomy.
Conclusion:
A literature review was performed using Pubmed, EMBASE and the Cochrane database for publications in the English language. MESH terms and keywords used included: osteoblastoma, osteoid osteoma, bone tumours, orbit, maxilla, zygoma, cranium. More than 50% of cases are found in patients younger than 30years old. An orbital location, particularly inferolateral, is highly unusual with only 19 adult and 44 paediatric case reports published detailing similar presentations – none involving the zygoma.
This is the first case of an orbito-zygomatic osteoblastoma.
CT and MRI imaging show classic lytic expansile lesions within a sclerotic shell and high T2 signal due to it’s vascularity. But the gold standard for a definitive diagnosis is pathological examination of the lesion.
Gross total resection is the management of choice to prevent malignant transformation and recurrence. Adjuvant radiotherapy has not shown clinically beneficial outcomes. MDT management with Maxillofacial, ENT (and often Neurosurgery) is essential.
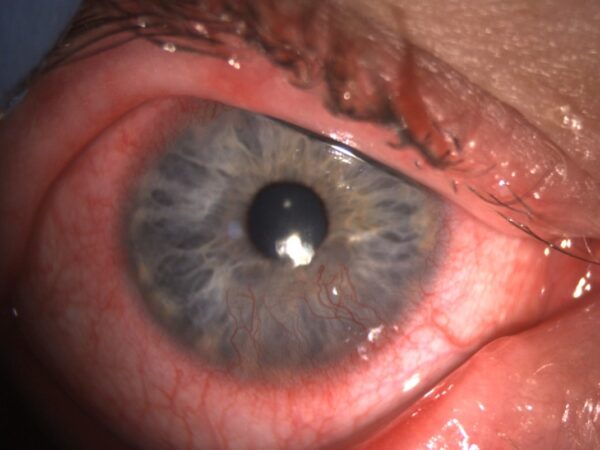
Case reports have shown the efficacy of 3D printing to allow more personalised preoperative planning and improved postop cosmetic outcome – could this be the future? In this case, no recurrence was identified after 6 months, and our patient has had a pleasing cosmetic outcome with no diplopia (shown below). He remains under review.
In conclusion, osteoblastoma should be considered as a differential diagnosis for orbital lesions that do not conform to the usual investigative histology or radiological imaging.



Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds