Management of Demodex Blepharitis in Clinical Practice
Blepharitis is one of the most common conditions presenting at ophthalmology and optometry clinics worldwide.1–3 It can affect patients of all ages and ethnicities.4 Traditionally the majority of blepharitis cases have been treated within ophthalmology departments. However, with the development of newer ocular hygiene products, and better training and information available, optometrists are becoming more adept and confident at treating minor eye conditions such as blepharitis. The clinical goal for practitioners is to identify the type of blepharitis, choose an effective treatment accordingly, and instruct and involve the patient in the long-term management of their condition.4
Demodex folliculorum and Demodex brevis (collectively referred to as Demodex) are microscopic, translucent, spindle-shaped ectoparasites; with a head, four pairs of legs and a long body tail (Figure 1); that live in the hair follicles and sebaceous glands of human skin. Demodex folliculorum (Figure 2), are slightly longer and typically reside in groups within the eyelash follicles. Demodex brevis (Figure 3), are smaller, often found in solitude, and generally reside deeper within the sebaceous and meibomian glands.
Demodex are photophobic5 and most active at night,6 travelling across the skin at a speed of up to 16 mm/hr.7 Feeding on skin cells and sebum, Demodex are most commonly found in areas rich in sebaceous glands such as our cheeks, nose, chin and the periocular area7,8; making the eyelids and eyelashes and ideal habitat.
Pathogenicity
Demodex mites have a complex role to play as microflora in our cutaneous ecosystem. The presence of the mites alone is not considered to be abnormal; their DNA has been found on 100% of people > 18 years of age.3 Nonetheless the pathogenic potential of Demodex remains widely debated.
Some suggest they are merely commensal organisms9–11: feeding on their host, without causing damage, but without purpose. It has also been proposed that there may be a mutualistic Demodex – host relationship, whereby Demodex ingest bacteria and other micro-organisms within the follicular canal, helping the host.9 The host’s immune system then regulates the quantity of Demodex present, preventing mite proliferation that could trigger an inflammatory response. However, if the quantity of Demodex increases beyond a ‘critical level’, they develop a pathogenic role, causing injury to the host.12,13 Thus, pro-inflammatory proteins are released, and the immune inflammatory response ensues with clinically visible cutaneous changes.9,12,14
It has also been suggested that Demodex are in fact opportunistic parasites: beginning as commensals, but have pathogenic potential in susceptible individuals.9 Although Demodex have been discovered on healthy individuals with no underlying conditions15,16; associations have been repeatedly made between an increased presence of Demodex and inflammatory conditions such as rosacea and blepharitis.13,17–20 It appears that the pathogenic potential of Demodex increases as the quantity of mites present increases.9,21
A further theory on the pathogenicity of Demodex is that they may act as vectors for bacteria. Researchers have begun to question whether it is not the presence of Demodex that causes problems, but whether the Demodex are ‘ill’.11 This hypothesis has arisen from the fact that treatment with tetracycline antibiotics resulted in clinical improvement of rosacea, even though the antibiotics had no effect on the Demodex quantities.6
Prevalence
Increasing age remains the most prevalent risk factor for Demodex infestation.18,22,23 It is believed that we acquire Demodex as children from older adults, and over the years the numbers of Demodex grow naturally as they continue to colonise. This results in a naturally higher prevalence of Demodex among older individuals.
Other studies have also indicated a link between ocular hygiene and age: suggesting that older individuals may have a reduced ability to clean the eyelids thoroughly, thus resulting in an increased prevalence of Demodex.18 This hypothesis was proposed when researchers found that the prevalence of Demodex was higher among younger individuals with poor eyelid hygiene, in comparison to older individuals with good eyelid hygiene.18
Clinical Manifestation
Symptomology
Demodex infestation exhibits symptoms similar to dry eye, as they both involve the ocular adnexa and manifest on the ocular surface; dryness, itch, irritation, burning sensation and foreign body sensation have all been recorded in the literature.17,19,20,22,24–26 While symptoms are subjective, and patient’s may report several symptoms, studies have found itch to be the symptom most significantly associated with Demodex infestation.19,20,26 However, Demodex can also be found in asymptomatic individuals.27
Signs
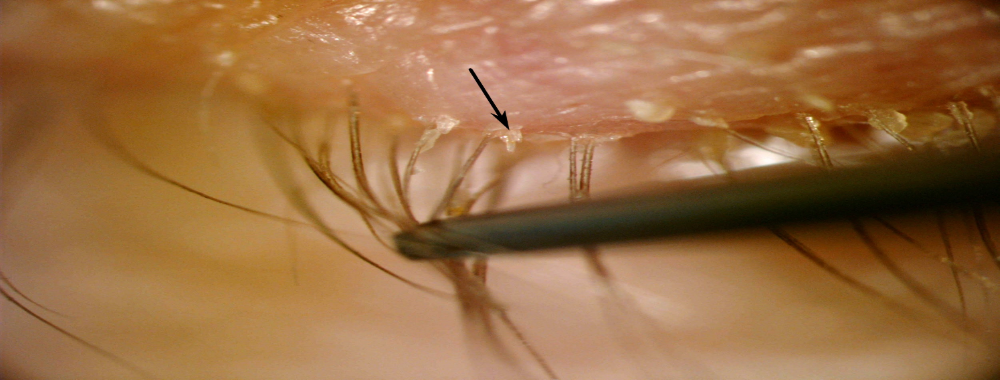
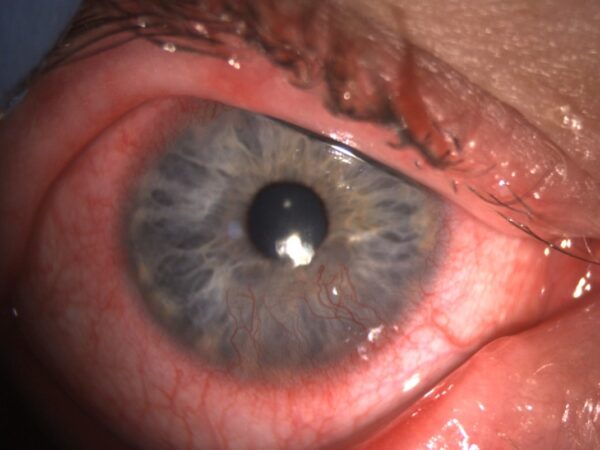
In susceptible individuals, the existence of Demodex causes direct damage to the anterior ocular structures.8,28 Cylindrical dandruff is believed to be caused by the abrasive movement of the mites within the eyelash follicles,28 or as an inflammatory cicatrix formed from dead mites within the follicle.29 Cylindrical dandruff, now considered a pathognomonic sign for presence of Demodex,30 can be differentiated from other ‘types of blepharitis collarettes’ by its distinctive appearance as a gelatinous collar at the base of the eyelash (Figure 4).28 By comparison, staphylococcal collarettes tend to be crusty sleeves, often stuck together, that can leave a bleeding ulcer when removed, and may be present anywhere along the length of the eyelash.31 Seborrheic collarettes are usually greasy and soft, they don’t leave a bleeding ulcer when removed, and are associated with seborrheic dermatitis.2,31
Chronic infestation of the eyelashes can also damage the follicles leading to lash disorders such as; mis-directed eyelashes, trichiasis or madarosis.25 Demodex brevis contribute to MGD by physically blocking and plugging the gland orifice, preventing the movement of lipids onto the tear film.21,28,32,33
Untreated persistent lid margin inflammation has been shown to spread to the conjunctiva and cause blepharoconjunctivitis that can prove resistant to conventional therapies25. However, Demodex targeted treatment has shown good ability to reduce ocular surface inflammation and irritation, suggesting Demodex may be an underlying cause of chronic blepharoconjunctivitis8,17,24,25,34.
Clinical Assessment
The following clinical procedure has been recommended when examining for the presence of Demodex.25,35
- Clinical history: Suspect Demodex; in patients with persistent blepharitis, conjunctivitis, keratitis; in younger patients with a history of blepharoconjunctivitis or recurrent chalazia that appear to be resistant to conventional treatments; in patients complaining of itchy eyes. Finally remember older patients, rosacea patients and contact lens wearers may be more susceptible to infestation.
- Slit lamp examination: After taking a thorough clinical history, examination of the eyelids and eyelashes using a slit-lamp is required. Be highly suspicious of Demodex infestation if cylindrical dandruff is present.
- Eyelash manipulation: It is possible to visualise Demodex on manipulation of the eyelash, without the need to remove the eyelash from the follicle.36,37 Although a standardised method has not been developed, it is suggested to choose an eyelash with cylindrical dandruff. Gently remove the cylindrical dandruff with a cotton bud/forceps. Using a sterile forceps, gently rotate the eyelash in clockwise and counter-clockwise directions to stimulate the Demodex to emerge from the eyelash follicle. If present, the Demodex tails will be visible as clear tubules emerging from the follicle (Figure 5). Although exact quantities of Demodex present cannot be obtained with eyelash manipulation alone, it is possible to confirm presence and to assess if there is a mild (≤ 3), moderate (4 – 6) or severe (≥ 7) infestation of the follicle.37
- Microscopic confirmation: Traditionally Demodex infestation was confirmed by removing the eyelash and counting the number of Demodex and eggs present on the epilated lash. This procedure is done by using sterile forceps to rotate the eyelash as described above. The lash is then epilated and placed on a microscope slide with a drop of alcohol and fluorescein, and the number of Demodex present is counted using a microscope. In clinical practice, eyelash epilation is not essential to accurately identify pathogenic Demodex infestation and Demodex blepharitis necessitating treatment.
Treatment
Current treatment methods for Demodex infestation recommended by the American Academy of Optometrists and College of Optometrists are to treat systemically with oral ivermectin or by topical application of 50% tea tree oil to the eyelids.4,38 However, tea tree oil is toxic to the ocular surface, irritating and uncomfortable for the patient, and needs to be applied weekly in-house by an expert clinician, resulting in increased chair-time and cost to the patient.43,44
Ivermectin is a broad-spectrum anti-parasitic drug primarily prescribed to treat human threadworm, and control river-blindness.39 It has been associated with several adverse reactions with varying degrees of severity, including but not limited to; diarrhoea, nausea, abdominal pain, hepatitis, headache, allergic reactions, ocular pain, fever 40–45. Caution is advised in the use of ivermectin by pregnant and nursing mothers, children and elderly individuals.39 It has not been well established whether older individuals respond differently to younger individuals, and in general there is an increased frequency of hepatic, renal, cardiac or concomitant disease and other drug therapy in elderly patients.39 The off-label use of ivermectin in the treatment of Demodex blepharitis has been successfully examined in clinical studies.46–48 However, there is a need to be cautionary when prescribing the drug, and potentially only consider when other treatment options have been unsuccessful.
There are several other methods of treatment that may be considered as first choice treatment in optometric clinical practice. Tea tree-based products such as face washes27 and lid wipes49 have shown to be effective at reducing signs and symptoms of Demodex blepharitis among affected individuals. The face wash can be administered as part of a lid scrub routine at home and can also be used on the entire face; therefore, theoretically treating Demodex present in hair follicles on the entire face, not just the eyelashes. The use of face wash as a baseline lid hygiene regimen is recommended in susceptible individuals.
The use of in-house microblepharoexfoliation, to help kickstart the cleaning regime and provide a deep-clean of the patients eyelids, has shown to give a greater improvement of the subjects’ symptoms of dry eye and blepharitis in comparison to the use of lid scrub treatments on their own.27
It has also been demonstrated that temperatures above 37 °C are damaging to Demodex.50 Higher temperatures cause death by protein coagulation and denaturation, and eventual paralysis of the Demodex nervous system.50 As such, treatments commonly used for MGD, such as intense pulsed light therapy51 and warm compresses52 have been shown to reduce Demodex quantities and help treat Demodex blepharitis.
Conclusion
Demodex blepharitis is commonplace to all optometric practices. It often presents with signs and symptoms similar to dry eye. It is possible to visualise Demodex in-situ on a slit lamp without the need to remove the eyelashes. Demodex blepharitis can be successfully treated in practice without the need for further referral for many patients. Consider an in-house deep clean of the eyelids to begin and advise patients on a suitable lid scrub routine and warm compresses for home use. Follow-up after one to two months depending on severity of infestation. In cases of chronic severe Demodex infestation with little to no improvement of signs and symptoms, consider referral for 50% tea tree oil treatment and/or combined treatment with a systemic intervention.
References
- Edwards RS. Ophthalmic emergencies in a district general hospital casualty department. Br J Ophthalmol. 1987;71:938-942.
- Nijm LM. Blepharitis: Classification. In: Holland E, Mannis M, Lee W, eds. Ocular Surface Disease: Cornea, Conjunctiva and Tear Film. Elsevier Inc.; 2013:55-60.
- Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocul Surf. 2009;7(2 Suppl):S1-S14. doi:10.1016/S1542-0124(12)70620-1
- Amescua G, Akpek EK, Farid M, et al. Blepharitis Preferred Practice Pattern®. Ophthalmology. 2018;126:P56-P93. doi:10.1016/j.ophtha.2018.10.019
- Spickett SG. Studies on Demodex folliculorum Simon (1842). I. Life history. Parasitology. 1961;51:181-192.
- Jarmuda S, O’Reilly N, Zaba R, Jakubowicz O, Szkaradkiewicz A, Kavanagh K. Potential role of Demodex mites and bacteria in the induction of rosacea. J Med Microbiol. 2012;61(PART 11):1504-1510.
- Rufli T, Mumcuoglu Y. The Hair Follicle Mites Demodex folliculorum and Demodex brevis : Biology and Medical Importance. Dermatologica. 1981;162:1-11.
- Coston T. Demodex folliculorum blepharitis. Trans Am Ophthalmol Soc. 1967;65:361-392.
- Lacey N, Ní Raghallaigh S, Powell FC. Demodex mites–commensals, parasites or mutualistic organisms? Dermatology. 2011;222(2):128-130.
- Baima B, Sticherling M. Demodicidosis revisited. Acta Derm Venereol. 2002;82(1):3-6.
- Elston DM. Demodex mites: Facts and controversies. Clin Dermatol. 2010;28(5):502-504.
- Georgala S, Katoulis AC, Kylafis GD, Koumantaki-Mathioudaki E, Georgala C, Aroni K. Increased density of Demodex folliculorum and evidence of delayed hypersensitivity reaction in subjects with papulopustular rosacea. J Eur Acad Dermatol Venereol. 2001;15(5):441-444.
- Forton F, Germaux M-A, Brasseur T, et al. Demodicosis and rosacea: Epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52(1):74-87.
- Kim JT, Lee H, Chun YS, Kim JC. Tear cytokines and chemokines in patients with Demodex blepharitis. Cytokine. 2011;53:94-99.
- Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case-control study using standardized skin-surface biopsy. Br J Dermatol. 1993;128(6):650-659.
- Thoemmes MS, Fergus DJ, Urban J, Trautwein M, Dunn RR. Ubiquity and diversity of human-associated Demodex mites. PLoS One. 2014;9(8):e106265. doi:10.1371/journal.pone.0106265
- Kheirkhah A, Casas V, Li W, Raju VK, Tseng SCG. Corneal Manifestations of Ocular Demodex Infestation. Am J Ophthalmol. 2007;143(5):743-749.
- Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between demodex and ocular discomfort. Invest Ophthalmol Vis Sci. 2010;51(6):2906-2911.
- Kabataş N, Doğan AŞ, Kabataş EU, Acar M, Biçer T, Gürdal C. The Effect of Demodex Infestation on Blepharitis and the Ocular Symptoms. Eye Contact Lens. 2017;43(1):64-67.
- Sędzikowska A, Osęka M, Grytner-Zięcina B. Ocular symptoms reported by patients infested with Demodex mites. Acta Parasitol. 2016;61(4):808-814.
- Lacey N, Kavanagh K, Tseng S. Under the lash: Demodex mites in human diseases. Biochem (Lond). 2009;31(4):2-6.
- Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Korean Med Sci. 2012;27(12):1574-1579.
- Roth AM. Demodex folliculorum in hair follicles of eyelid skin. Ann Ophthalmol. 1979;11(1):37-40.
- Gao YY, Di Pascuale MA, Elizondo A, Tseng SC. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007;26(2):136-143.
- Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505-510.
- Kojima T, Ishida R, Sato EA, et al. In Vivo Evaluation of Ocular Demodicosis Using Laser Scanning Confocal Microscopy. Invest Ophthalmol Vis Sci. 2011;52:565-569.
- Murphy O, O’Dwyer V, Lloyd-McKernan A. The efficacy of tea tree face wash, 1, 2-Octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Contact Lens Anterior Eye. October 2017. doi:10.1016/j.clae.2017.10.012
- English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91(3):362-372.
- Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303-312. doi:10.1007/s10792-016-0249-9
- Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089-3094.
- Efron N, Efron N. Eyelash disorders. Contact Lens Complicat. January 2012:67-75. doi:10.1016/B978-0-7020-4269-0.00007-9
- Desch C, Nutting WB. Demodex folliculorum (Simon) and D. brevis Akbulatova of Man: Redescription and Reevaluation. J Parasitol. 1972;58(1):169. doi:10.2307/3278267
- Randon M, Liang H, El Hamdaoui M, et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol. 2015;99(3):336-341. doi:10.1136/bjophthalmol-2014-305671
- Liang L, Safran S, Gao Y, Sheha H, Raju VK, Tseng SCG. Ocular Demodicosis as a Potential Cause of Pediatric Blepharoconjunctivitis. Cornea. 2010;29(12):1386-1391. doi:10.1097/ICO.0b013e3181e2eac5
- Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15(3):539-574. doi:10.1016/j.jtos.2017.05.001
- Mastrota KM. Method to Identify Demodex in the Eyelash Follicle Without Epilation. Optom Vis Sci. 2013;90(6):e172-e174. doi:10.1097/OPX.0b013e318294c2c0
- Murphy O, O’ Dwyer V, Lloyd-McKernan A. The clinical use of eyelash manipulation in the diagnosis of Demodex folliculorum blepharitis. Eye Contact Lens. 2019;In Press.
- The College of Optometrists. Blepharitis (Lid Margin Disease). Clinical Management Guidelines. https://www.college-optometrists.org/guidance/clinical-management-guidelines/blepharitis-lid-margin-disease.html. Published 2018. Accessed June 1, 2018.
- Food and Drugs Administration. STROMECTOL ®. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/050742s026lbl.pdf. Published 2009. Accessed May 23, 2017.
- Chouela EN, Abeldaño AM, Pellerano G, et al. Equivalent therapeutic efficacy and safety of ivermectin and lindane in the treatment of human scabies. Arch Dermatol. 1999;135(6):651-655.
- De Sole G, Remme J, Awadzi K, et al. Adverse reactions after large-scale treatment of onchocerciasis with ivermectin: combined results from eight community trials. Bull World Health Organ. 1989;67(6):707-719.
- Heukelbach J, Winter B, Wilcke T, et al. Selective mass treatment with ivermectin to control intestinal helminthiases and parasitic skin diseases in a severely affected population. Bull World Health Organ. 2004;82(8):563-571. doi:/S0042-96862004000800005
- Pacqué M, Munoz B, Taylor H., Dukuly Z, Greene B., White A. Safety of and compliance with community-based ivermectin therapy. Lancet. 1990;335(8702):1377-1380. doi:10.1016/0140-6736(90)91253-7
- Sparsa A, Bonnetblanc J-M, Peyrot I, Loustaud-Ratti V, Vidal E, Bédane C. [Systemic adverse reactions with ivermectin treatment of scabies]. Ann Dermatol Venereol. 2006;133(10):784-787.
- Thomas J, Peterson GM, Walton SF, Carson CF, Naunton M, Baby KE. Scabies: An ancient global disease with a need for new therapies. BMC Infect Dis. 2015;15(1). doi:10.1186/s12879-015-0983-z
- Filho PAN, Hazarbassanov RM, Grisolia ABD, Pazos HB, Kaiserman I, Gomes JÁP. The efficacy of oral ivermectin for the treatment of chronic blepharitis in patients tested positive for Demodex spp. Br J Ophthalmol. 2011;95(6):893-895. doi:10.1136/bjo.2010.201194
- Holzchuh FG, Hida RY, Moscovici BK, et al. Clinical Treatment of Ocular Demodex folliculorum by Systemic Ivermectin. Am J Ophthalmol. 2011;151(6):1030-1034.e1. doi:10.1016/j.ajo.2010.11.024
- Salem DA-B, El-Shazly A, Nabih N, El-Bayoumy Y, Saleh S. Evaluation of the efficacy of oral ivermectin in comparison with ivermectin-metronidazole combined therapy in the treatment of ocular and skin lesions of Demodex folliculorum. Int J Infect Dis. 2013;17(5):e343-7. doi:10.1016/j.ijid.2012.11.022
- Cheng AM, Sheha H, Tseng SC. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol. 2015;26(4):295-300. doi:10.1097/ICU.0000000000000168
- Zhao YE, Guo N, Wu LP. The effect of temperature on the viability of Demodex folliculorum and Demodex brevis. Parasitol Res. 2009;105(6):1623-1628. doi:10.1007/s00436-009-1603-x
- Zhang X, Song N, Gong L. Therapeutic Effect of Intense Pulsed Light on Ocular Demodicosis. Curr Eye Res. October 2018:1-7. doi:10.1080/02713683.2018.1536217
- Murphy O, O’ Dwyer V, Lloyd-Mckernan A. The Efficacy of Warm Compresses in the Treatment of Meibomian Gland Dysfunction and Demodex Folliculorum Blepharitis. Curr Eye Res. 2019. doi:10.1080/02713683.2019.1686153
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds