Rosai-Dorfman disease: a rare cause of bilateral lacrimal gland swelling
Abstract
A 31-year-old systemically well Asian male presented with a 3-month history of painless, progressive bilateral lacrimal gland swelling associated with lymphadenopathy. Bloods revealed elevated eosinophils, erythrocyte sedimentation rate and hypergammaglobulinaemia consistent with non-specific inflammation. Magnetic resonance imaging found bilateral lacrimal enlargement and cervical lymphadenopathy. Supraclavicular lymph node biopsy revealed follicular hyperplasia with no evidence of malignancy. Lacrimal gland biopsy revealed dense infiltrate of histiocytes, lymphocytes, and plasma cells. Extended histology review and analysis made the diagnosis of Rosai-Dorfman disease, also known as sinus histiocytosis with massive lymphadenopathy. The patient made a good recovery with systemic immunosuppression. This case highlights the importance of multi-disciplinary input and communication to reach a diagnosis. Ruling out neoplastic, infectious and inflammatory aetiology is essential in all cases of uni- or bilateral facial swelling of unclear aetiology.
Case Presentation
A 31-year-old Asian male initially presented to an otolaryngologist with a 3-month history of left-sided presumed parotid gland swelling, associated with painless, progressive bilateral lacrimal gland swelling. There was no loss of function, such as difficulty chewing, swallowing or visual changes. Systemically he was well with no constitutional upset. Past medical history included tonsillitis requiring tonsillectomy and gastric reflux disease for which he took omeprazole. There was no recent travel history or infectious history.
Otolaryngology examination described a patient of a healthy weight and normal observations. They detected two non-tender small lumps over the angle of the left mandible consistent with mild parotid lymph node enlargement. Laryngopharynx examination was normal, so he was subsequently referred to the ophthalmic department.
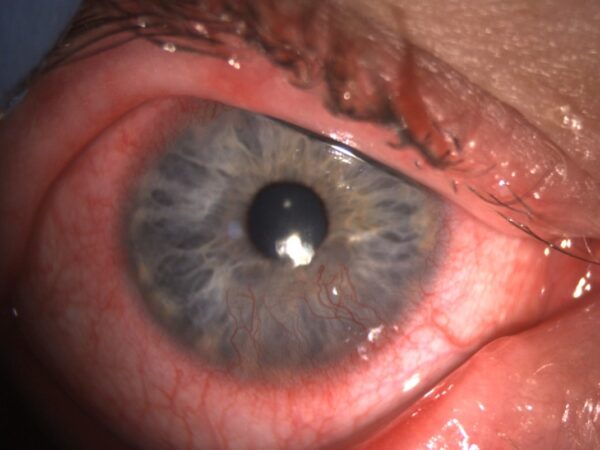
Ocular examination revealed firm, uniform, non-tender swelling of both upper eyelids, with S-shaped deformities to both lid contours, consistent with enlarged lacrimal glands.[Figure 1] There were no rashes or skin changes across the face or eyelids. Ocular motility was normal and there was no clinical proptosis. Vision was excellent, with normal pupillary responses and healthy posterior segments.
Given the bilateral nature of his lacrimal gland enlargement, it was deemed likely that there was a systemic aetiology. Therefore, the differentials at presentation were neoplastic, infectious or inflammatory disease.
Investigations
Baseline bloods revealed elevated eosinophils 0.7 (normal 0-0.4 10*9/L), proteins 84 (normal 57-76g/L) globulins 41 (normal 18-32g/L) and erythrocyte sedimentation rate 60 (normal 0-10mm/hour) (ESR), while electrophoresis revealed hypergammaglobulinaemia. Collectively these results were consistent with a non-specific infectious or inflammatory response.
Lactate dehydrogenase was within normal limits. Serum infectious screens, including tuberculosis, borreliosis, toxoplasmosis, syphilis, human immunodeficiency virus, cytomegalovirus and Epstein-Barr virus, were all negative. Serum rheumatoid factor was elevated at 32.8 (normal 0-15 IU/L) and anti-nuclear antibody (ANA) was positive. Furthermore, immunoglobulins -A, -E and -G were elevated at 3.3, 360 and 23.4 respectively (normal reference range IgA 0.8-2.8 g/L, IgE: 0-100 kU/L, IgG: 6-16 g/L). Serum angiotensin converting enzyme, thyroid function tests and TSH-receptor antibodies, were within normal limits. The remaining connective tissue autoantibody screen was unremarkable.
Magnetic resonance imaging (MRI) revealed parotid glands of normal size with enlarged parotid lymph nodes. There was bilateral, symmetrical lacrimal gland enlargement with uniform signal intensity and mild enhancement with no focal mass lesion.[Figure 2] The rest of the globe, optic nerve and extraocular muscular appearances were normal. In summary, there was bilateral diffuse lacrimal gland enlargement with bilateral peri-parotid, cervical and superior mediastinal lymphadenopathy.[Figure 3] The radiological differential included sarcoidosis and lymphoma.
Given the mediastinal changes, a chest x-ray was arranged which revealed an enlarged, globular cardiac outline, this was later confirmed on echocardiography as a mild right-sided pericardial effusion with diastolic collapse of the right ventricle but no haemodynamic compromise. Cardiology opinion was that there was no primary cardiac abnormality causing this multi-system presentation, with continued monitoring to ensure no deterioration.
Meanwhile, a core biopsy of his right supraclavicular lymph node was undertaken and revealed non-specific reactive changes with follicular hyperplasia and marked reactive plasmacytosis. A small proportion was IgG4-positive. There was no evidence of lymphoproliferative malignancy or granuloma, and mycobacteria testing was negative. A second opinion at a tertiary unit was obtained and whilst they agreed with the initial report, but a unifying histopathological diagnosis was still not evident. To correlate with the biopsy, an immunoglobulin-G profile was obtained which revealed significantly elevated IgG1 of 28 (normal 2.2-10.8 g/L) and elevated IgG3 of 3.42 (normal 0.05-0.9 g/L) but only a slightly elevated IgG4 of 2.7 (normal 0-2.4 g/L).
After 7 months of investigation without a diagnosis, the patient then began to develop shortness of breath, fatigue and palpable neck lymphadenopathy. Rheumatology reviewed the patient and organised a positive emission tomography (PET) scan, which revealed widespread lymphadenopathy with a continued suspicion of lymphoma. The patients’ eosinophil count then inexplicably normalised on repeat samples whilst the ESR elevated to a peak of 114mm/hr. Rheumatology suggested a lacrimal gland biopsy could potentially elucidate ambiguities with the initial nodal biopsy.
Lacrimal gland biopsy revealed dense infiltrate of histiocytes, lymphocytes and plasma cells. Abundant plasma cells were found on immunohistochemistry, most were IgG with a small proportion IgG4 secreting. No atypical cells and no granulomas were seen. The histiocyte rich inflammation raised the suspicion of Rosai-Dorfman disease (RDD). A further excisional lymph node biopsy was obtained given the rarity of lacrimal gland associated RDD, which confirmed the diagnosis.
Differential diagnoses
This interesting clinical picture initially had two possible differential diagnoses. The first was the rare diagnosis of Kimura disease (KD), or eosinophilic hyperplastic lymphogranuloma, which was first suggested by the patient himself. KD is a poorly understood eosinophilic inflammatory disease that usually effects the subcutaneous, lymphatic and glandular tissue of the face, head and neck. In one case review, they found around 200 case reports worldwide, highlighting the scarcity of this disease. Key features which bolster KD are the patients’ gender, ethnic origin and age, as well as fulfilling the classic triad of serum eosinophilia, elevated serum IgE, and follicular hyperplasia on biopsy. However, eosinophils normalised without treatment which go against this diagnosis. Furthermore, a normal renal function goes slightly against this diagnosis, as glomerulonephritis and/or deranged electrolytes coexists in up to 60% of KD.
KD can be safely observed if there is little impact on function. With systemic upset or widespread lesions immunosuppression treatment, such as corticosteroids or ciclosporin, have been utilised with variable success. Localised lesions can be surgically excised if it is safe to do so. Eosinophilia, as discussed, can bring about numerous problems and these must be examined by the appropriate specialist, in our case this was a cardiologist.
The second differential was immunoglobulin G4-related disease (IgG4-RD), features that align with this diagnosis include the painless, uniform bilateral lacrimal swelling, associated pericardial effusion and the lymph node biopsy having a degree of IgG4 positivity. But only a small proportion of the biopsy was IgG4 positive (less than 40%) and there was no storiform fibrosis or obliterative phlebitis, which are hallmark pathology findings in IgG4-RD. Furthermore, the subsequent lacrimal gland biopsy continued display equivocal evidence, with few IgG4 plasma cells seen on biopsy and on bloodwork.
More unlikely differentials include Mikulicz syndrome and Sjögren’s syndrome, as although there is abnormal enlargement of the lacrimal glands, there is a distinct lack of symptoms such as dry eye, dry mouth or swallowing difficulties. Furthermore, typically lymph tissue is not involved in Mikulicz or Sjogren related diseases.
Treatment, outcome and follow up
Initially, given the painless nature of the swelling with no loss of functionality, including no haemodynamic compromise on echocardiography, the patient continued to work as a GP trainee without any specific treatment other than active observation.
However, with increasing fatigue and shortness of breath, he was commenced on oral prednisolone by rheumatology once a neoplastic process was relatively confidently ruled out. Following the eventual diagnosis of RDD, 10 months since initial presentation, methotrexate was added to his treatment regime by a histiocytosis specialist. Lacrimal gland swelling fully resolved, his cervical lymphadenopathy improved clinically and radiographically, while his constitutional systems improved substantially.[Figure 4] He suffered no overt side effects from immunosuppressive therapy.
Discussion
Patients with lacrimal gland swelling can present with varied symptoms, these include a noticeable change in appearance of the orbit, eyelid or skin, pain, eye watering, blurred vision, double vision and/or ptosis. Signs and symptoms are commonly unilateral, and in bilateral cases a systemic pathology should be suspected.
A full ophthalmic examination should be undertaken, including assessment of optic nerve function, ocular motility and exophthalmometry. Classic features of lacrimal gland enlargement include an S-shaped lid deformity and upon eversion of the upper eyelid, lacrimal gland tissue is visibly enlarged. Depending on aetiology, cicatricial eyelid changes or profound erythema can be present.
Investigation of lacrimal gland swelling has three broad pathways based on aetiology, that being neoplasia, infectious or inflammation. Serum markers can equip the clinician with rapid clues. An abnormal blood count can reveal haematological malignancy. Serum infectious screens have high sensitivity for detecting multiple bacterial and viral pathogens. ESR and C-reactive protein (CRP) can indicate inflammatory processes. An array of autoimmune diseases can be included, or excluded, based on clinical correlated serum markers. Orbital imaging can display characteristic diagnostic features, such as the bony involvement in adenoid cystic carcinoma or the well-circumscribed borders in pleomorphic adenoma.
Biopsy is often gold standard to obtaining a diagnosis, as was the case in our patient. Caution should be applied, as incisional biopsy is not appropriate in specific situations, for example if pleomorphic adenoma is suspected, here the tumour should be removed en bloc. It is not uncommon to obtain a second opinion on histology or harvest multiple biopsies if there is continued diagnostic uncertainty. This bolsters confidence in a diagnosis and the safety of instigating treatment, especially when utilising immunosuppressive drugs which could significantly exacerbate the clinical picture. In our patient, both the lymph node and lacrimal gland biopsy reports were relatively ambiguous in attempting to clarify the inflammatory process and required tertiary centre histology opinions. Therefore, a third biopsy was obtained, allowing further analysis to confirm the diagnosis.
Treatment of lacrimal gland swelling is dependent on the varied aetiology, which often requires multiple subspecialty input, for example oncology with neoplastic disease or infectious diseases in borreliosis. In cases where lacrimal gland swelling causes morbid proptosis leading to corneal exposure and/or optic nerve compromise, urgent ophthalmic input may be required. This can involve temporary tarsorrhaphy, lateral canthotomy or orbital decompression.
Rosai-Dorfman disease
RDD, also known as sinus histiocytosis with massive lymphadenopathy, is a form of histiocytosis. This is a group of rare diseases characterised by an abnormal increase in the number of specialist white blood cells known as histiocytes. They play a key role in phagocytic tissue repair and immune system regulation. The definitive aetiology of RDD remains unknown, many have postulated BRAF mutations while others have attributed an infectious agent such as Epstein-Barr virus, herpes virus and more recently COVID-19.
The typical clinical presentation of RDD is painless, progressive lymph node enlargement in a child or young adult. Uncommonly non-specific illness, fatigue or weight loss are accompanied. Laboratory features include a raised ESR, hypergammaglobulinaemia (both seen in 90%) and rarely raised rheumatoid factor and/or ANA positivity. All four of these features were observed in our patient. Nearly 90% have bilateral cervical lymphadenopathy, with other lymph nodes sites infrequently involved. Extranodal involvement has been reported to occur in nearly any system and can mimic significant diagnoses such as meningioma or lymphoma. In one registry of 423 patients, 43% had at least one site of extranodal involvement plus lymph node involvement, while there were 23% had extranodal involvement only.
Typical histology reveals heterogenous, non-cancerous proliferation of lymphocytes and enlarged histiocytes that typically display immunoreactivity with S-100 and/or CD68, our patient was indeed positive for both of these markers. There is usually an absence of necrosis, granuloma, and atypia. Another distinctive histological feature of RDD, again present in our patient, is emperipolesis – a phenomenon whereby intact lymphocyte cells are found in histiocyte intracytoplasmic vacuoles, thus escaping proteolytic degradation.
Ophthalmic involvement is a common site to be affected, but this is still infrequent, observed in only 11% of cases in one series. Reported manifestations include orbital masses, uveitis, scleritis, serous retinal detachments, choroidal effusions and lacrimal gland enlargement.
RDD is a self-limiting in up to 50% of cases, and so patients can be safely observed for spontaneous resolution upon diagnosis. However, in those with a protracted clinical course, constitutional upset or reduced function, treatment may be warranted. Given the rarity of the disease, there is no defined treatment protocol, however treatments are usually immunosuppressive. Corticosteroids are frequently utilised, along with steroid-sparing treatments including mycophenolate, cladribine and methotrexate reported. Radiotherapy has been used in some case reports.
In those with RDD related orbital masses, surgery may be required. In a study of 76 patients presenting to an ophthalmic clinic with RDD, they observed 4 orbital masses (5.3%) which all required an orbitotomy. Interestingly, none of the 76 patients had lacrimal gland enlargement, highlighting the scarcity of its involvement in RDD.
Learning Points
- Rosai-Dorfman disease a rare cause of lacrimal gland enlargement.
- The expert opinion and communication between multiple specialities is often required to clinch uncommon diagnoses.
- Obtaining multiple biopsies and specialist histopathology opinion is key when there is no clear initial tissue diagnosis.
- In any case of unilateral or bilateral glandular swelling, neoplastic disease must be ruled out.
References
- Rajesh A, Prasanth T, Naga Sirisha VC, Azmi M. Kimura’s disease: A case presentation of postauricular swelling. Niger J Clin Pract. 2016; 19(6):827-830. doi: 10.4103/1119-3077.164361.
- Priyokumar OS, Niteshore MS, Ratan K. Bilateral Kimuras disease with sinusitis and parotid gland involvement: A case report and a brief review of literature. IOSR J Dent Med Sci. 2014; 13:22‑5.
- Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol. 1969; 87(1):63-70.
- Gulwani H, Bhalla S, Srivastava A. Isolated lacrimal gland involvement in Rosai-Dorfman-Destombes disease. Indian J Ophthalmol. 2008; 56(6):507-9. doi: 10.4103/0301-4738.43375.
- Gaitonde S. Multifocal, extranodal sinus histiocytosis with massive lymphadenopathy: an overview. Arch Pathol Lab Med. 2007; 131(7):1117-21. doi: 10.5858/2007-131-1117-MESHWM.
- Paulli M, Rosso R, Kindl S, Boveri E, Marocolo D, Chioda C, et al. Immunophenotypic characterization of the cell infiltrate in five cases of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease). Hum Pathol. 1992; 23(6):647-54. doi: 10.1016/0046-8177(92)90320-3.
- Foucar E, Rosai J, Dorfman RF. The ophthalmologic manifestations of sinus histiocytosis with massive lymphadenopathy. Am J Ophthalmol. 1979; 87(3):354-67. doi: 10.1016/0002-9394(79)90077-1.
- Lee-Wing M, Oryschak A, Attariwala G, Ashenhurst M. Rosai-Dorfman disease presenting as bilateral lacrimal gland enlargement. Am J Ophthalmol. 2001 May;131(5):677-8. doi: 10.1016/s0002-9394(00)00864-3.
- Reddy A, Beigi B, Linardos E. Rosai-Dorfman syndrome affecting the lacrimal gland. Orbit. 2001 Sep;20(3):239-242. doi: 10.1076/orbi.20.3.239.2625.
- Choi MB, Salomão DR, Smith WM, Pulido JS, Garrity JA. Ophthalmic Findings of Rosai-Dorfman Disease. Am J Ophthalmol. 2018; 188:164-172. doi: 10.1016/j.ajo.2018.01.037
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds



