A Congress Meeting: BOPSS 2024
The British Oculoplastic Surgery Society (BOPSS) was founded in 2000 by world-renowned oculoplastic surgeons TO create a collaborative forum for advancing the field of oculoplastic surgery in the United Kingdom and Ireland.. The society was established with the vision of promoting excellence in education, research, and clinical practice in this highly specialised area. Over the years, BOPSS has grown to become a cornerstone of the oculoplastics community, bringing together surgeons from across the world who are dedicated to improving patient outcomes through innovation and shared expertise.
This year’s British Oculoplastic Surgery Society annual meeting was held in the vibrant and bustling city of Leeds from 19th to 21st June 2024, and it was nothing short of fantastic. It was hosted at The Carriageworks Theatre – an elegant, architecturally stunning venue in the heart of this cosmopolitan city. The meeting spanned three days, each with a distinct focus:

Day 1: Update & Recent Advances Day
The opening day featured sessions on eyelid disorders, lacrimal disorders, orbital disorders, and aesthetic oculoplastic surgery. Keynote lectures included Professor Don Kikkawa’s update on paediatric ptosis and Professor Bob Goldberg’s insights into the latest techniques in aesthetic oculoplastic surgery.
Day 2: Scientific Programme
The second day commenced with free paper presentations, followed by a keynote lecture by Professor Don Kikkawa on how technology enhances oculofacial surgery.

Afternoon sessions included a round table discussion, a trainee quiz on ophthalmic dermatology, and additional free paper presentations. The day concluded with a keynote by Professor Bob Goldberg on staged surgical rehabilitation for thyroid-related orbitopathy.
Day 3: Scientific Programme
The final day began with free paper sessions, followed by a keynote lecture by Professor Bob Goldberg on the latest techniques in aesthetic oculoplastic surgery. Afternoon sessions focused on orbit-related topics, including sclerotherapy for orbital vascular disease and the role of interventional radiology in orbital conditions. The meeting concluded with the Annual General Meeting for full members.
Professor Bob Goldberg:
- Professor Bob Goldberg, MD, FACS, the world-renowned oculoplastic virtuoso from UCLA With a blend of unparalleled expertise and effortless charm, he made even the trickiest eyelid procedures sound as straightforward as brewing a perfect cup of tea—milk in last, naturally (because some things are non-negotiable).
- Professor Bob Goldberg emphasised the critical role of “TPS” (tarsal platform show) and “BFS” (brow fat span) in achieving harmonious eyelid aesthetics, noting that asymmetry in TPS is far more noticeable than BFS. Highlighting the power of ptosis surgery, he explained how manipulating skin crease height—even creating a subtle “cosmetic micro ptosis”—can achieve symmetry that patients are so acutely aware of.
- Professor Goldberg also delved into techniques for enhancing TPS visibility, such as judicious removal of orbital fat from the brow pad and adding volume to the superior orbit using fillers or free fat grafts. Fillers in the eyebrow fat pad, he explained, not only maintain volume but also preserve aesthetic balance.
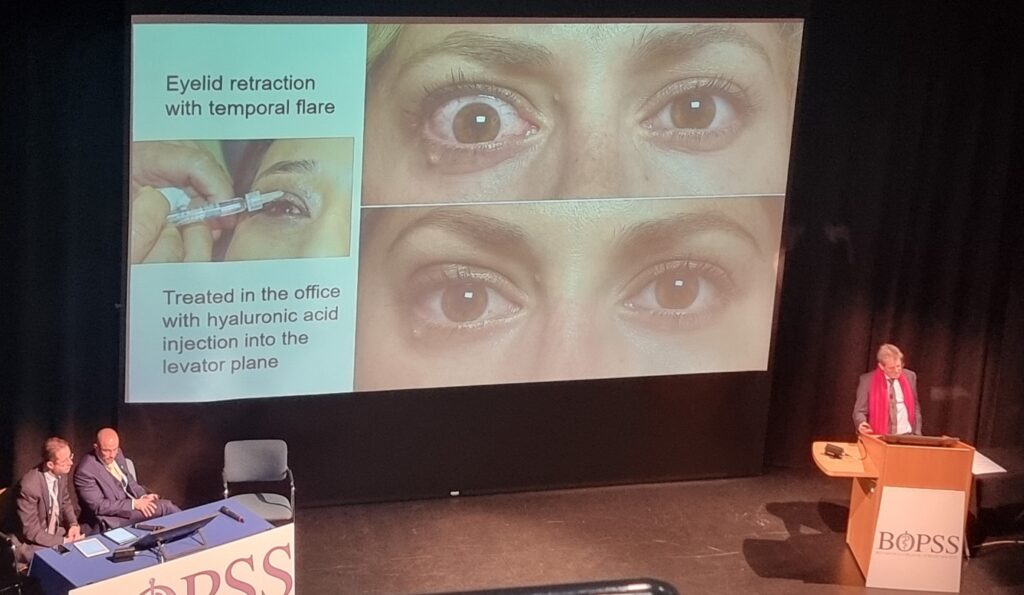
- A pioneer in aesthetic reconstructive surgery for thyroid eye disease, he shared invaluable strategies for managing eyelid retraction with temporal flare, including injecting hyaluronic acid into the levator plane to restore fullness. He warned against aggressive fat removal in thyroid eye disease patients to avoid accentuating proptosis and advised under correcting eyelid retraction to prevent secondary ptosis.
Professor Don Kikkawa:
- Professor Don Kikkawa, MD, FACS, is a world-renowned expert in paediatric oculoplastics, with decades of experience in managing ptosis and a surgical resume that could rival a riveting Tolstoy novel. Based at the University of California, San Diego, he brought his trademark wit and wisdom to an enlightening lecture on paediatric ptosis management, blending clinical expertise with an engaging touch of humour.
- Diving straight into the challenges of super maximal levator resection for congenital ptosis, Professor Kikkawa candidly addressed the 25% re-operation rate associated with the procedure, proving that even the best techniques come with their hurdles. He explained that the second-line options include a silicone sling, a frontalis flap, or repeating the super maximal levator resection. While a frontalis flap can be effective, he quipped that achieving symmetry in severe cases can sometimes feel like chasing the holy grail of oculoplastics.
- He went on to detail minimally invasive techniques that reduce recovery times while preserving eyelid function, showcasing surgical refinements that deliver excellent outcomes with less downtime. The audience was left brimming with ideas, practically vibrating with excitement, and promptly swarmed him during the coffee break like bees around a particularly knowledgeable flower, all desperate for a few more golden tips.
- Professor Kikkawa’s emphasis on early intervention in congenital ptosis struck a chord, as he stressed the importance of timely diagnosis and treatment to prevent amblyopia and support normal visual development.
Professor Radoslaw Rozycki:
- Professor Radoslaw Rozycki, an eminent figure in oculoplastic and lacrimal surgery, is based in Warsaw, Poland, where he leads the charge in advancing minimally invasive techniques.
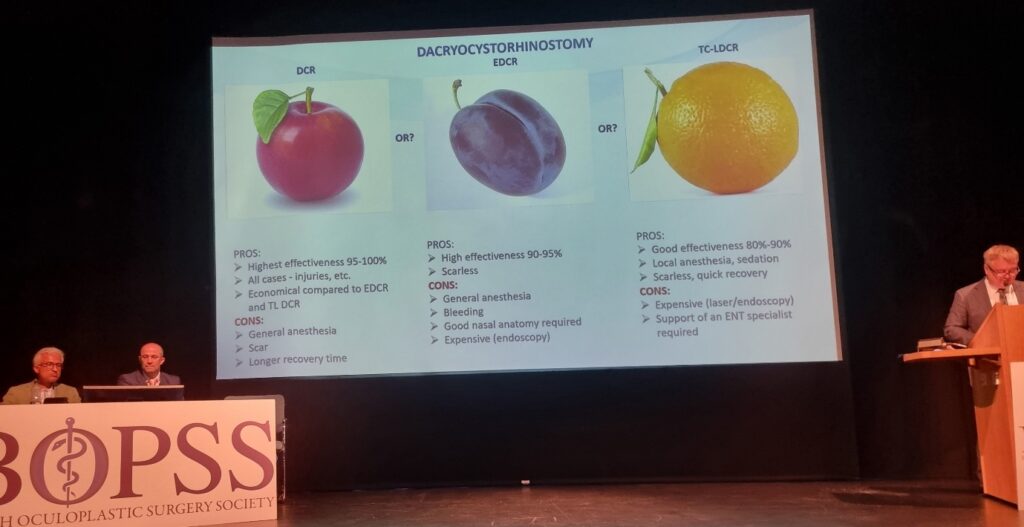
- At the BOPSS 2024 meeting, Professor Rozycki delivered a compelling lecture on Transcanalicular Laser Dacryocystorhinostomy (TC-LDCR), a cutting-edge procedure transforming the management of nasolacrimal duct obstructions. Known for his ability to blend rigorous technical detail with real-world insights, he provided a comprehensive view of this innovative approach, cementing its role as a game-changer in lacrimal surgery.
- TC-LDCR is a minimally invasive technique that uses a fine laser fibre inserted through the punctum to create a passage from the lacrimal sac into the nasal cavity. By avoiding external incisions, the procedure offers significant aesthetic and functional advantages over traditional external dacryocystorhinostomy (DCR). This precision-guided technique is complemented by endoscopic visualisation, ensuring accuracy and safety throughout the procedure.
- Professor Rozycki presented data demonstrating success rates comparable to, and in some cases exceeding, those of external DCR. Recent studies report patency rates of over 90%, validating TC-LDCR as a reliable first-line treatment for suitable patients. He noted that the procedure is particularly effective in cases of primary acquired nasolacrimal duct obstruction, with excellent long-term outcomes.
- A major advantage of TC-LDCR is its reduced risk of complications. By avoiding external incisions, the technique minimises scarring, infection risks, and damage to surrounding structures. This makes it an attractive option for patients concerned about cosmetic outcomes or those with higher surgical risk profiles.
- Patient experience was a recurring theme in Professor Rozycki’s talk. He highlighted how TC-LDCR significantly shortens recovery times, reduces postoperative discomfort, and eliminates the need for visible scars, leading to higher satisfaction rates. In an era where patient-centric care is paramount, these outcomes align perfectly with modern healthcare priorities.
- Professor Rozycki also discussed the evolving role of TC-LDCR within the broader spectrum of lacrimal surgery. He cautioned against using it indiscriminately, stressing the importance of thorough patient evaluation and understanding its limitations, such as in cases of extensive scarring or anatomical abnormalities.
- With his characteristic humour, Professor Rozycki quipped that the most challenging part of TC-LDCR isn’t the surgery itself but convincing patients it’s not science fiction. He left us questioning what we liked most in terms of our taste in fruit (see below) and reckoned the same analogy with DCR approaches. In truth, his ability to make the futuristic feel accessible is precisely why he remains a global leader in this ever-evolving field.
My Ponderings:
As a regular delegate of BOPSS meetings since my Foundation Year 2 training, I have always valued the unique combination of education, debate, and collaboration these gatherings foster. The 2024 meeting in the diverse city of Leeds was particularly engaging, with a strong focus on aesthetic oculoplastics that sparked lively discussions among consultants from different countries, reflecting the diverse approaches to this evolving field. I was particularly struck by the new techniques shared for staple operations such as ptosis correction and blepharoplasty, especially the nuanced challenges faced in single-creased eyelids. The meeting also highlighted exciting research into upcoming treatments for thyroid eye disease, promising to further reduce the need for, the often dreaded, decompression surgery. Discussions on the use of fillers to restore volume to the eyebrow fat pad or levator plane in stable thyroid eye disease patients with lid retraction offered innovative, patient-focused solutions that I will consider in my own practice moving forward.
Quick Must-Know Highlights From the Meeting:
As someone well-practised in the art of writing notes at speed—complete with the quintessential “doctor’s handwriting” that might require a hieroglyphic key to decipher—I still managed to scribble down a few stellar points and tips from the meeting. These pearls of wisdom, I hope, will be of some use to my oculoplastic colleagues, whether you’re an aspiring medical student, a hardworking resident, or a seasoned consultant looking for a tip or perhaps even a helpful reminder!
- In cases of upper lid retraction blepharotomy procedure, if lateral flare is present, release the lateral horn of the levator and if severe, recess the levator and suture the tarsus to the levator and advance the suture out to the skin crease to allow for adjustment.
- In graded blepharotomies, perforate the conjunctiva and muller’s muscle centrally and laterally to leave a central strand present. Never perforate medially.
- Orbital decompression is the preferred surgical method to improve lower lid retraction in thyroid eye disease.
- Sebaceous gland carcinoma can masquerade as unilateral blepharitis/ mimic a chalazion or present as a lacy pattern across the conjunctiva with pagetoid spread in 50%. Biopsy needs to be a full thickness lid sample for higher sensitivity.
- Sebaceous gland carcinoma has a high mortality rate and needs monitoring for 10 years.
- Use the BLICK pneumonic for examining epiphora: Blink dynamics, Lid malposition, Imbrication of skin, Conjunctival chalasis, Kissing puncti.
- Propranolol, for orbital vascular disease, is not effective after the child is 1 years old but works well if taken consistently in the fast growth phase of the lesion.
- If a child presents with an orbital cellulitis that bleeds, consider lymphatic malformation or rhabdomyoscarcoma as differentials.
- Ptosis surgery is the most powerful tool to control skin crease height
- Hyaluronic filler in the levator plane is useful in lid retraction.
- Teprotumumab works well for protoptosis and diplopia in acute and chronic thyroid eye disease but is not as effective in lid retraction and dry eye.
- If lateral wall decompression is undertaken, there is a risk of “hourglass” deformity laterally due to loss of volume and temporalis wasting.
- Lateral wall decompression gains 7mls of orbital volume, on average.
- Sclerotherapy is the management of choice for low-flow venous malformations.

Conclusion:
In summary, the talks were both informative and thought-provoking, offering a chance to revisit teachings from previous meetings while sparking intrigue about the potential of artificial intelligence in oculoplastics—from diagnostics to surgical planning. These discussions may or may not have left me pondering my future role in an AI-driven world, potentially as useful as a trapdoor on a canoe. That said, they instilled a glimmer of hope that, given enough time, machines might truly become humanity’s best friend (second only to dogs, of course) and allow surgeons to achieve even more optimised results for their patients.
The networking opportunities were equally rewarding—catching up with colleagues and friends from hospitals near and far, debating papers, and marvelling at the impressive posters crafted by residents and fellows. Their hard work and dedication were a testament to the passion that drives our specialty. The meeting in Leeds was a vibrant celebration of the innovation, collaboration, and sheer enthusiasm that define the oculoplastics community.
Lastly, I’d like to offer my congratulations to the well-deserved winners of BOPSS 2024:
- Video Prize: Christine Putri (Sheffield) for “Treading the LINES: A facial reconstruction challenge.
- Free Paper Prize: Holly Clarke (Portsmouth) for “Cemiplimab, a programmed cell death 1 (PD1) protein inhibitor for the treatment of locally advanced and metastatic cutaneous squamous cell carcinoma of the head and neck – real world data.”
- E-Poster Prize: Harry Rosen (Queen Alexandra Hospital) for “How to create 3D models of orbital structures from dissected human body donors.”
- TEDct Prize John Vekinis (Imperial College) for “A ‘Real life’ study of thyroid eye disease (TED) following radioactive iodine (RAI) therapy”
Looking forward to seeing you at the next BOPSS meeting in Brighton, 2025!

HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds