Microbial keratitis
Introduction
Microbial keratitis is an infective condition that affects the cornea (the clear window of the eye). The usual cause is contact lens wear, but infection of the cornea can also result from exposure of the eye (for example if the eyelids are not blinking normally), loss of sensation in the eye surface, injury or surgery, lack of tears (dry eye), and in people whose immune system is not functioning properly. The usual cause is bacterial, but some cases are due to fungal infection.
It is a serious condition and is a major cause of corneal opacity and loss of vision worldwide (Kaye 2017). An estimated 2.0–3.5 million cases of bacterial keratitis are reported annually. But these data are considered significantly lower than the actual incidence rate due to underreporting from the developing world (Singh et al 2022).
It usually begins suddenly with redness and pain in one eye. The eye waters and there may be a discharge. Light may hurt the eye, making it difficult to open. The vision of the eye may be blurred.
Topical antimicrobial therapy is a critical component in its management (Kaye 2017) and more serious cases will need to be referred on the same day to the ophthalmologist. In the UK in England alone, there are over 2700 in-patient hospital episodes with suspected corneal infection per annum (Moussa et al., 2021). In the USA approximately 70,000 cases are diagnosed annually (Lin 2019).
There are several different types of microbial keratitis including:
Clinical Evaluation
Bacterial Keratitis | Herpes Simplex Keratitis | Herpes Zoster Ophthalmicus | Fungal Keratitis | Acanthamoeba keratitis | |
Risk Factors | Contact lens wear is the biggest risk factor, and it has been found that the incidence of bacterial keratitis is 4–5 times higher in contact lens wearers compared to non-wearers (Carnt 2017) The main risk factors for MK in a contact lens wearer are: · increased days of wear · poor hygiene (hand, lens and storage case) · younger age · male gender · smoking · buying contact lenes from the internet · ocular surface disease, including: · corneal exposure · corneal decompensation · chronic epithelial defect · neurotrophic keratopathy, e.g. secondary to HSK or diabetes · ocular trauma or surgery · immune compromise · topical steroid use · lid margin infection (which is usually Staphylococcal) | Herpes Simplex is associated with · poor general health · immunodeficiency · fatigue · Systemic or topical steroids, or other immunosuppressive drugs · There are also other possible aggravating factors such as · sunlight (UV) · fever · extreme heat or cold · infection (systemic or ocular) · trauma (ocular) Any history of previous ocular herpes simplex attacks can be a significant feature in the diagnosis of the condition. | Herpes Zoster · This mainly occurs in healthy patients between the ages of 40 to 60. · It is thought that up to 1/3 of cases occur in patients under the age of 50 · It may also occur with immune compromise such as HIV/AIDS and medical immunosuppression | The main risk factors for fungal keratitis are injuries from vegetative matter | Acanthamoeba keratitis is rare in the general population (estimated annual incidence: 1.4 per million per annum It is much more common in contact lens wearers. The majority of Acanthamoeba keratitis cases (71-91%) are linked to contact lens wear Mostly this is soft lenses and more particularly if it is continuous wear or reusable wearing schedules It may also be linked to · Inadequate disinfection · The use of non-sterile contact lens solutions · Using tap water to rinse contact lenses or the storage case · Bacteria and fungi can also contaminate the storage case which results in a biofilm where acanthamoeba can grow and thrive · As acanthamoeba is present in water, exposure to shower, pool, or hot tub water can lead to infection · In the UK, higher incidence is found in hard water districts and where bathrooms are supplied by tank-stored water. |
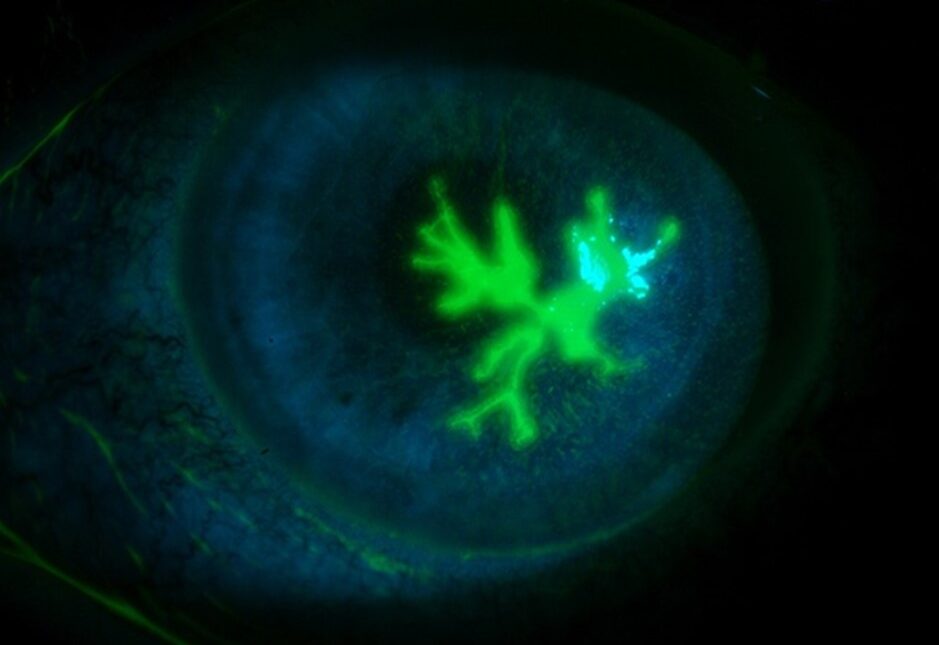
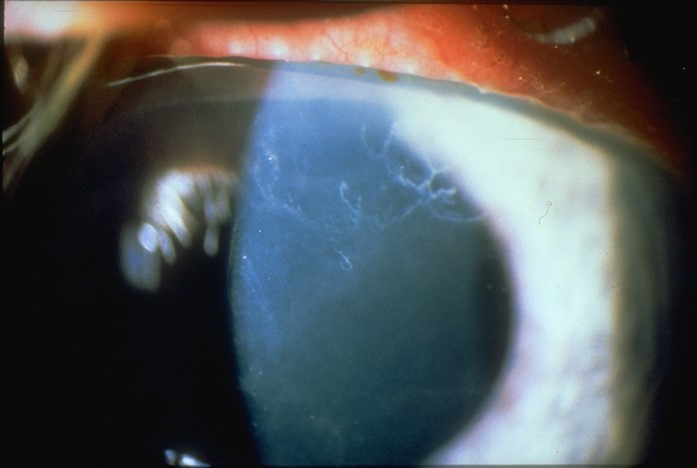
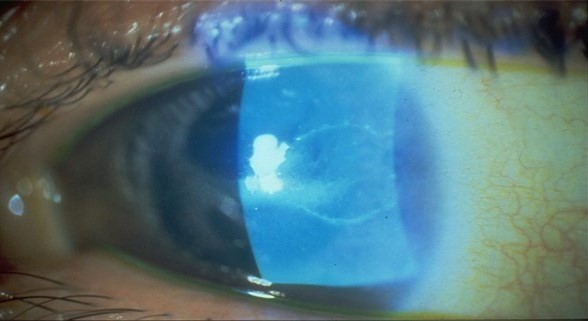
Clinical Presentation | · Sudden onset painful red eye with rapid progression · Reduced vision Signs · Lid swelling · Epiphora · Discharge · Conjunctival redness · Corneal lesion (note the position and depth) · Bacterial infections typically form circular ulcers · Anterior chamber activity · Possible hypopyon Symptoms · Pain which can vary from moderate to severe · Redness · Photophobia · Discharge · Blurred vision · Usually unilateral | · These may be variable but usually an acute onset unilateral red eye with pain and reduced vision Signs · In the early stages superficial punctate keratitis may be seen · This progresses to form a dendritic ulcer which may be single or multiple and have terminal end bulbs (not seen in pseudodendrites) · If enlargement continues a geographic ulcer may develop Symptoms · Patient reports discomfort which can range from foreign body sensation to pain · Blurred vison · Epiphora · Redness Usually unilateral, but may be bilateral in atopic patients | · It mainly affects patients in their 50s and 60s but can occur at any age and may be linked to immune compromised patients. · Unilateral painful rash Signs Skin: · Unilateral red rash on forehead and upper eyelid. Crusting developing after 2-3 weeks. · Swelling around lid and orbit which may cause the eyelids to close · Hutchinson’s sign is involvement of the tip of the nose. This indicates nasociliary involvement and often signifies ocular complications too Ocular · Mucopurulent conjunctivitis · Episcleritis · Scleritis · Keratitis · Epithelial: consisting of superficial punctate keratitis and pseudo dendrites · Stromal: nummular keratitis with anterior stromal deposits · Disciform: endotheliitis with a disc of corneal oedema · Neurotrophic: Corneal nerve damage can cause a persistent epithelial defect Symptoms · General malaise · Fever · Headache · Pain · Altered sensation on one side of forehead Rash appears any time between 1 day to one week later | · Sudden onset painful red eye with rapid progression · Reduced vision Signs · Lid swelling · Epiphora · Discharge · Conjunctival redness · Corneal lesion (note the position and depth) · Fungal infections typically form circular ulcers · Anterior chamber activity · Possible hypopyon Symptoms · Pain which can vary from moderate to severe · Redness · Photophobia · Discharge · Blurred vision · Usually unilateral | · Sudden onset painful red eye with rapid progression · Reduced vision Signs · Lid swelling · Epiphora · Discharge · Conjunctival redness · Corneal lesion (note the position and depth) · Acanthamoeba may initially show a dendritic pattern, and later showing a disciform ulcer · Anterior chamber activity · Possible hypopyon Symptoms · Pain which can vary from moderate to severe · Redness · Photophobia · Discharge · Blurred vision · Usually unilateral |
Investigation | · Full anterior segment examination to look at lids, conjunctiva and cornea of both eyes to exclude other causes · Check for size and depth of any corneal lesion Test corneal sensitivity (can indicate neurotrophic conditions such as herpetic disease | · Full anterior segment examination to exclude other causes · Posterior chamber examination to check for herpetic retinitis · Diagnosis is usually made on clinical features · If it is uncertain swab for viral or other microbial causes (Acanthamoeba may be misdiagnosed as herpes simplex) o Both conjunctival and corneal swabs may be taken | · Careful anterior segment examination to exclude other causes · Posterior segment examination to check for secondary complications (see below) | Full anterior segment examination to look at lids, conjunctiva and cornea of both eyes to exclude other causes Check for size and depth of any corneal lesion Test corneal sensitivity (can indicate neurotrophic conditions such as herpetic disease) Anterior chamber examination to check for cells and flare | · Full anterior segment examination to look at lids, conjunctiva and cornea of both eyes to exclude other causes · Check for size and depth of any corneal lesion · Test corneal sensitivity (can indicate neurotrophic conditions such as herpetic disease) · Anterior chamber examination to check for cells and flare |
Management & Advice
Bacterial Keratitis | Herpes Simplex Keratitis | Herpes Zoster Ophthalmicus | Fungal Keratitis | Acanthamoeba keratitis | |
Overview | This is an emergency and immediate referral to ophthalmology is required If the ulcer is bigger than 1mm or within 3mm of the centre of the cornea it should be referred same day as an emergency There may also be anterior chamber activity Most hospital units perform a corneal scrape and culture or PCR to guide therapy If the patient wears contact lenses, it is important to send lenses, case and any solutions for culture | Herpes simplex virus (HSV) infection is very common. Usually latent
· Treatment is with topical antiviral Meticulous follow up and appropriate SOS advice is important as this is a potentially sight threatening disease
| Herpes zoster ophthalmicus (HZO) is caused by localized reactivation of varicella zoster virus (VZV) in ophthalmic division of the trigeminal nerve
| This is an emergency and immediate referral to ophthalmology is required
| This is an emergency and immediate referral to ophthalmology is required
|
Non-pharmacological | There are no non-pharmacological interventions for bacterial keratitis | There are no non-pharmacological interventions for herpetic keratitis | There are no non-pharmacological interventions for herpetic keratitis | There are no non-pharmacological interventions for fungal keratitis | There are no non-pharmacological interventions for acanthamoeba keratitis |
Pharmacological | Treatment will be intense (hourly) topical broad-spectrum antibiotic plus mydriatic for photophobia or severe pain
| Epithelial herpes simplex keratitis is usually treated with topical antiviral agents (Tabbara 2005)
| This should be referred urgently to hospital if there is deep corneal stroma involvement, raised IOP or risk of corneal perforation
| Firstly as for bacterial keratitis scrape and culture is carried out before commencing intense treatment
| Diagnosis of this is normally confirmed by histology (corneal scrape) and culture or PCR
|
Self Care | As contact lens wear is the biggest risk factor for bacterial keratitis good patient hygiene and compliance is essential to minimise the risk | This condition may recur and patients should be advised to seek urgent attention if it does | The patient may be advised to o Rest o Ensure they have a good diet o Take plenty of fluids, and o Avoid contact with those who are elderly or pregnant, babies and children who haven’t been exposed to VZV, or people who are immunodeficient | N/A | As contact lens wear is the biggest risk factor for acanthamoeba keratitis good patient hygiene and compliance is essential to minimise the risk as well as avoiding contact with water |