Beyond the Ocular Surface: How Nutrition and Lifestyle Shape Dry Eye Disease
A closer look at how nutrition, systemic health, and integrative care intersect in dry eye management.
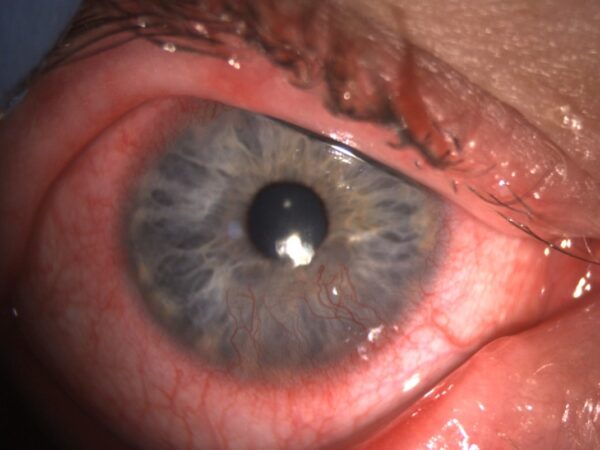
Dry eye disease (DED) is increasingly recognized not just as a localized ocular surface disorder, but as a multifactorial condition influenced by systemic health. Nutrition, inflammation, mitochondrial function, and even the gut microbiome all play roles in its pathophysiology. At its core, DED involves chronic inflammation, oxidative stress, and tear film instability, but a growing body of evidence highlights how nutritional status can amplify or mitigate these mechanisms.1,2,3
For eye care providers, this opens an important opportunity: integrating dietary and lifestyle assessments into clinical care to improve outcomes and offer patients a more comprehensive management plan.
Can Nutritional Deficiencies Play a Role in Dry Eye?
The TFOS DEWS III and TFOS Lifestyle Report, along with recent reviews, underscore how Western-style diets, low in antioxidants and essential fatty acids but high in processed foods, exacerbate oxidative stress and inflammation, worsening DED.2,3,4 By contrast, nutrient-rich, Mediterranean-style diets appear protective, offering synergistic benefits that extend beyond any single supplement.
This means clinicians should think broadly. While supplementation with specific vitamins or essential fatty acids can be effective in cases of deficiency, the strongest evidence favors a whole-diet, lifestyle-integrated approach that supports ocular surface health alongside systemic wellness.3,4
Integrating lifestyle and dietary assessments into clinical care may improve outcomes and allow for more comprehensive and integrative management of DED. To better understand this connection, the following sections will review the evidence on how specific nutrient deficiencies, both macronutrients such as essential fatty acids and micronutrients including vitamins and minerals, contribute to ocular surface dysfunction and disease progression. We will also examine emerging data on the role of botanical compounds with anti-inflammatory and antioxidant properties, as well as the influence of the gut microbiome on ocular surface health. Together, these factors highlight how nutrition and systemic health intersect with dry eye management, offering new opportunities for more personalized and effective care.
Essential Fatty Acids (Macronutrients)
Omega-3 fatty acids, particularly EPA and DHA from fish, flaxseed oil, and algae, are the most studied fats in relation to DED. Their metabolites, resolvins and protectins, help resolve ocular inflammation by reducing leukocyte infiltration, enhancing macrophage activity, and supporting epithelial repair. These pathways improve tear secretion, corneal nerve health, and tear film stability. Evidence from TFOS DEWS II, the TFOS Lifestyle Report, and TFOS DEWS III consistently shows that low omega-3 intake, coupled with high omega-6 consumption, tilts the inflammatory balance and may worsen DED.1,2,3
Populations at risk include patients consuming Westernized diets with low fish intake, vegans without supplementation, and those with fat malabsorption disorders (celiac disease, Crohn’s disease, ulcerative colitis, pancreatic insufficiency, or post-bariatric surgery). Beyond the eye, omega-3s are well known to reduce cardiovascular risk and support cognitive health.
While many omega-6 fatty acids promote inflammation, gamma-linolenic acid (GLA), found in borage oil and evening primrose oil, has anti-inflammatory effects. GLA enhances prostaglandin E1 production, which supports tear secretion and meibomian gland function. Clinical trials show that supplementation with EPA, DHA, and GLA improves tear production and reduces dry eye symptoms, even in highly symptomatic patients.2,4 At the systemic level, GLA has demonstrated benefits in conditions such as rheumatoid arthritis and atopic dermatitis, reinforcing its broader immune-modulating role.
Omega-7 fatty acids, particularly palmitoleic acid from sea buckthorn oil, are an emerging area of research. Studies suggest anti-inflammatory and antioxidant effects, with benefits for lipid layer stability, meibomian gland function, and relief of evaporative dry eye symptoms.2,4,5 Omega-7s may also support mucosal membrane integrity and metabolic health, with potential roles in improving insulin sensitivity and cardiovascular function.
Palmitoleic acid has been shown to preserve tear secretion by reducing inflammation in the lacrimal gland (Nakamura et al, 2017); and has shown to attenuate seasonal spikes in tear film osmolarity in individuals with dry eye (Larmo et al, 2010).
Importantly, essential fatty acids cannot be synthesized by the human body and must be obtained through diet. A Mediterranean-style dietary pattern, rich in fish and olive oil, provides omega-3s alongside moderate omega-6 intake, which supports meibomian gland function, stabilizes the tear film, and reduces obstruction.2,4 For patients whose intake may be inadequate, measuring the serum omega-3 index can offer an objective way to assess status. This biomarker reflects long-term dietary intake and absorption and can guide practitioners in recommending targeted supplementation when dietary sources are insufficient.
Vitamins and Minerals (Micronutrients)
Deficiencies in the following vitamins have been identified to contribute or exacerbate dry eye disease.
Vitamin A is indispensable for mucin production, epithelial repair, and goblet cell function, making it a cornerstone of ocular surface integrity. Deficiency can lead to conjunctival keratinization, xerophthalmia, reduced tear production, and, in severe cases, blindness.1,4 While severe deficiency is uncommon in developed countries, it should still be considered in at-risk populations such as patients with bariatric surgery, chronic alcohol use, liver disease, or highly restrictive diets4. Dietary sources include retinol-rich animal foods (liver, egg yolks, dairy, oily fish) and beta-carotene–rich vegetables (carrots, spinach, sweet potatoes). In the context of dry eye disease, oral supplementation may improve tear quality when deficiency is present, whereas topical formulations have shown more consistent benefits in enhancing tear stability and ocular surface health.1
Vitamin B12 is vital for DNA synthesis, nerve function, and cellular repair. Deficiency may manifest as ocular discomfort, burning, or neuropathic-like eye pain6. At-risk groups include vegans, older adults, those on acid-suppressing or GLP-1 medications, and patients with malabsorptive gastrointestinal disorders.3 Supplementation has been shown to reduce neuropathic ocular pain and improve dry eye signs such as Schirmer scores, TBUT, and tear clearance.6,3 Both systemic supplementation and topical B12 (often with hyaluronic acid) have demonstrated benefits.
Vitamin D exerts immunoregulatory effects on the ocular surface, down-modulating NF-κB–dependent cytokines (e.g., IL-1β, IL-6, TNF-α) and supporting epithelial barrier integrity—via locally expressed vitamin D receptors and activating enzymes identified in corneal epithelium, ciliary body, and retinal tissues.7 Vitamin D metabolites have been detected in ocular fluids, and serum 25(OH)D remains the best status marker.7 Clinically, low 25(OH)D has been associated with reduced TBUT and Schirmer scores, increased tear osmolarity, and greater symptom burden; a meta-analysis reports lower serum vitamin D levels in DED and links deficiency to worse signs and symptoms.7 Systemic supplementation, particularly in deficient or refractory patients, has improved tear secretion, stability (TBUT), osmolarity, and symptoms, and may potentiate the effects of topical lubricants.7 Practical considerations include confirming deficiency with serum 25(OH)D, recognizing risk groups (limited sun exposure, darker skin, obesity, malabsorption, and chronic systemic disease), and appreciating that dose–response is nonlinear and baseline-dependent; co-ingestion with dietary fat can enhance absorption.7 In population guidance, Mediterranean-style dietary patterns complement supplementation strategies and broader ocular surface care.4,7
Vitamin C is a potent antioxidant that neutralizes oxidative stress, supports collagen synthesis in the cornea and conjunctiva, and promotes epithelial healing1. While overt deficiency is rare, risk groups include those with poor fruit and vegetable intake, smokers, heavy alcohol use, or chronic gastrointestinal disease.4 In DED, vitamin C supplementation helps reduce inflammation and support ocular tissue repair, making it a valuable adjunct.
Vitamin E is a fat-soluble antioxidant that stabilizes cell membranes and protects tear film lipids from oxidative damage.1 It supports lacrimal and meibomian gland function and reduces cytokine-driven inflammation. Though rare, deficiency can occur with fat malabsorption syndromes, liver disease, or restrictive diets.4 Supplementation, particularly topical or liposomal forms, has been shown to enhance corneal healing and reduce symptoms.4
Botanical Antioxidants
Plant-based compounds also provide adjunctive support. Curcumin (turmeric) reduces inflammatory cytokines and promotes neurotrophic factors, though bioavailability-enhanced formulations are often required. Green tea extract (EGCG) improves meibomian gland function and suppresses inflammatory mediators. Bilberry (anthocyanins) enhances tear production, while red ginseng reduces ocular surface inflammation.4 These botanicals are best viewed as complementary to, not replacements for, foundational nutritional strategies.
Mitochondrial Health and Oxidative Stress
Mitochondrial dysfunction has emerged as a central driver in DED. Excess mitochondrial reactive oxygen species (mtROS) contribute to oxidative stress, epithelial barrier disruption, goblet cell loss, and inflammatory signaling. Recent studies describe mitochondrial oxidative stress, apoptosis, and mtDNA damage as pivotal mechanisms of ocular surface instability, suggesting that mitochondria may represent a novel therapeutic target.8,9
Preclinical studies show that alpha-lipoic acid (ALA) and coenzyme Q10 (CoQ10) reduce apoptosis, protect neurons, and improve ATP production, while antioxidant combinations with vitamin E amplify these effects.8.9 Clinically, CoQ10, ALA, and related nutraceuticals are being evaluated as adjunct therapies for DED.9
From a lifestyle perspective, promoting mitochondrial resilience through exercise, sleep, and Mediterranean-style diets rich in antioxidants may reduce systemic oxidative burden and support ocular health.
What is the Current Evidence on Gut Microbiome and Dry Eye?
Emerging research highlights the gut–eye axis as a contributor to DED. Patients with Sjögren’s syndrome show profound gut dysbiosis, including reduced diversity, lower Firmicutes/Bacteroidetes ratios, and reduced beneficial bacteria such as Bifidobacterium and Faecalibacterium, correlating with disease severity.10 Even in non-autoimmune dry eye, shifts such as increased Veillonella and decreased Subdoligranulum have been observed.10
This supports the concept of a gut dysbiosis–ocular surface–lacrimal gland axis, where microbial imbalance can exacerbate systemic immune dysregulation, impair tear production, and promote ocular surface inflammation.10,11 Early studies of probiotics, prebiotics, and microbiome-focused diets suggest potential benefits in restoring microbial balance and alleviating symptoms. However, addressing gut dysbiosis often requires a broader, integrative approach—optimizing diet quality while also incorporating lifestyle factors such as stress management, regular physical activity, and adequate sleep, all of which influence both gut and ocular surface health.
How Can Clinicians Integrate Nutrition and Lifestyle into Practice?
Dry eye disease is multifactorial and closely tied to systemic health. Clinicians can integrate evidence-based nutrition and lifestyle guidance with a simple, repeatable approach:
- Expand the history: In addition to medications and systemic conditions, assess diet patterns, hydration, sleep quality, stress load, physical activity, and environmental/screen exposures—using specific, targeted questions.
- Make it actionable: Provide resources on simple Mediterranean-style targets patients can follow (e.g., fish/seafood 2–3 times per week, vegetables and fruit at every meal aiming for 5+ servings daily, and beans/legumes and nuts several times per week). Ask patients to complete a 3–7-day food and fluid journal and review it at follow-ups to spot patterns and choose 1–2 concrete next steps.
- Use evidence-based nutraceutical strategies: Prioritize a food-first approach, and when dietary intake is insufficient or inconsistent, consider targeted supplementation to support essential fatty acids and key micronutrients. When clinically indicated, use targeted nutrient testing to personalize recommendations and collaborate with integrative specialists to guide individualized care.
- Take an integrative view: Address key lifestyle drivers—sleep, stress regulation, physical activity, hydration, and environmental/screen habits—as foundational supports for immune and nervous system balance, alongside ocular therapies to improve dry eye outcomes and overall health.
- Stay current: Engage with reputable, evidence-based continuing education and professional communities focused on ocular wellness and nutrition—such as the Ocular Wellness & Nutrition Society—to help keep guidance aligned with the evolving evidence base.
With dry eye disease emerging as a growing burden for patients and a persistent challenge for clinicians, there is a clear opportunity to close the gap between symptomatic treatment and long-term control. By recognizing the “missing link” of nutrition and systemic health—and applying evidence-based dietary and lifestyle strategies—eye care providers can adopt a whole-body approach that not only stabilizes the ocular surface and reduces flares but also supports overall health and wellbeing.
References
- Bron AJ, de Paiva CS, Chauhan SK, Bonini S, Gabison EE, Jain S, Knop E, Markoulli M, Ogawa Y, Perez V, Uchino Y, Yokoi N, Zoukhri D, Sullivan DA. TFOS DEWS II Pathophysiology Report. Ocul Surf. 2017;15(3):438–510.
- Craig JP, Alves M, Wolffsohn JS, Downie LE, Efron N, Galor A, Gomes JAP, Jones L, Markoulli M, Stapleton F, Starr CE, Sullivan AG, Willcox MDP, Sullivan DA. TFOS Lifestyle Report. Ocul Surf. 2023;30:240–253.
- Stapleton F, Argüeso P, Asbell P, Azar D, Bosworth C, Chen W, Ciolino J, Craig JP, Gallar J, Galor A, Gomes JAP, Jalbert I, Jie Y, Jones L, Konomi K, Liu Y, Merayo-Lloves J, Oliveira FR, Quinones VAP, Rocha EM, Dogru M. TFOS DEWS III Digest Report. Am J Ophthalmol. 2025;S0002-9394(25)00276-4.
- Bhandarkar NS, Shetty K, Narendra P, Kiran A, Shetty R, Shetty KB. Nutrition and diet for dry eye disease: Insights toward holistic management. Indian J Ophthalmol. 2024;72(10):1412–1423.
- Larmo PS, Järvinen RL, Setälä NL, Yang B, Viitanen MH, Engblom JR, Tahvonen RL, Kallio HP. Oral sea buckthorn oil attenuates tear film osmolarity and symptoms in individuals with dry eye. J Nutr. 2010;140(8):1462–1468.
- Ozen S, Ozer MA, Akdemir MO. Vitamin B12 deficiency evaluation and treatment in severe dry eye disease. Graefes Arch Clin Exp Ophthalmol. 2017;255(6):1173–1177.
- Rolando M, Barabino S. Dry Eye Disease: What Is the Role of Vitamin D? Int J Mol Sci. 2023;24(2):1458.
- Xia Y, Zhang Y, Du Y, Wang Z, Cheng L, Du Z. Comprehensive dry eye therapy: combating inflammation, oxidation, and mitochondrial damage. J Nanobiotechnol. 2024;22(1):233.
- Ouyang W, Yan D, Hu J, Liu Z. Multifaceted mitochondria as a novel therapeutic target in dry eye: insights and interventions. Cell Death Discov. 2024;10(1):398.
- Moon J, Yoon CH, Choi SH, Kim MK. Can Gut Microbiota Affect Dry Eye Syndrome? Int J Mol Sci. 2020;21(22):8443.
- Song J, Dong H, Wang T, Yu H, Yu J, Ma S, Song X, Sun Q, Xu Y, Liu M. What is the impact of microbiota on dry eye: a gut-eye axis review. BMC Ophthalmol. 2024;24(1):262.
- Nakamura S, Kimura Y, Mori D, Imada T, Izuta Y, Shibuya M, Sakaguchi H, Oonishi E, Okada N, Matsumoto K, Tsubota K. Restoration of Tear Secretion in a Murine Dry Eye Model by Oral Administration of Palmitoleic Acid. Nutrients. 2017 Apr 5;9(4):364. doi: 10.3390/nu9040364. PMID: 28379171; PMCID: PMC5409703.
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds
