Progression of Eye Disease over seven years in a patient with X-linked Chronic Granulomatous Disease on Blood derived allogenic tears and Anakinra therapy
Introduction
Chronic Granulomatous Disease (CGD) is a primary immunodeficiency, which affects phagocytes of the innate immune system. As a result, it greatly increases susceptibility to bacterial and fungal infections. It is a relatively uncommon condition. CGD is normally diagnosed in infancy and has an incidence of between 1 in 200,000 and 1 in 250,000 live births[i].
Infections of the lung, skin lymph nodes and liver are the most frequent manifestations of CGD[ii]. Patients are usually placed on long term antifungal and antibiotic medications. Since the introduction of antifungals, particularly Itraconazole the mortality in CGD has plunged. It is relatively common to have ocular manifestations as a result of CGD, with documented reports of chorioretinitis and focal subretinal granuloma[iii].
Case
A 26-year-old male initially was diagnosed as a child with X-linked CGD after initially presenting to hospital with a neck abscess. The patient was then placed on long term antibiotic prophylactic therapy. His initial main complaints were of acne, associated skin abscesses, and obesity. The patient did not suffer any notable systemic infections. Definitive management in the form of a bone marrow transplant was considered. However, no matched donor was found, and it was decided against pursuing a higher risk mismatched donor.
The patient first presented to ophthalmology at 19-years-old after referral from his community optometrist with the complaint of ocular surface inflammation and dry eye. At this time, he had evidence of Meibomian gland dysfunction, ocular surface inflammation and peripheral corneal vascularisation in both eyes, more marked left than right. Visual acuity was 6/9 right eye and 6/38 left eye. The patient was commenced on Doxycycline and given oral lubricants. This provided a positive outcome, and the patient was told to continue Doxycycline 100mg once a day in the long-term.
At the age of 21 years the patient then had several presentations spanning a four year period relating to flare-ups of ocular surface inflammation and vascularisation of the left cornea. (Figure 1) To treat this inflammation the patient was prescribed a tapering regimen of systemic steroids, preservative free topical steroids, lubricants and antibiotics.
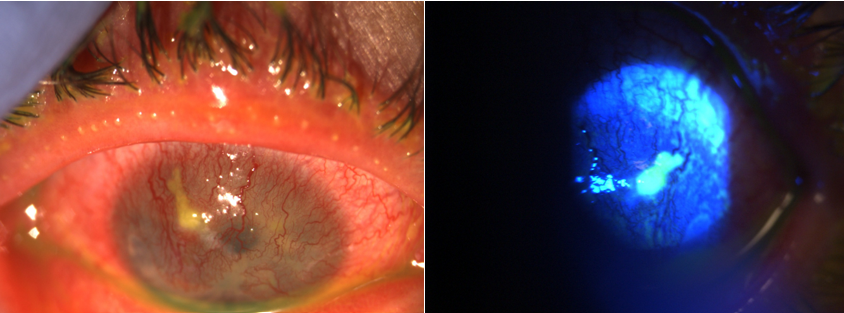
At 23-years-old the patient had been continuing treatment as above. However, aggressive inflammation had led to complete corneal vascularisation in the left eye. The left eye was amblyopic and the patient was not aware of progressive vascularisation. There was also new vascularisation in the right eye (not involving visual axis). He then developed a descemetocele and micro perforation. As a result of progressive inflammation he was commenced on blood derived allogeneic tears. The micro perforation was treated conservatively without the need of corneal glue or surgical intervention.
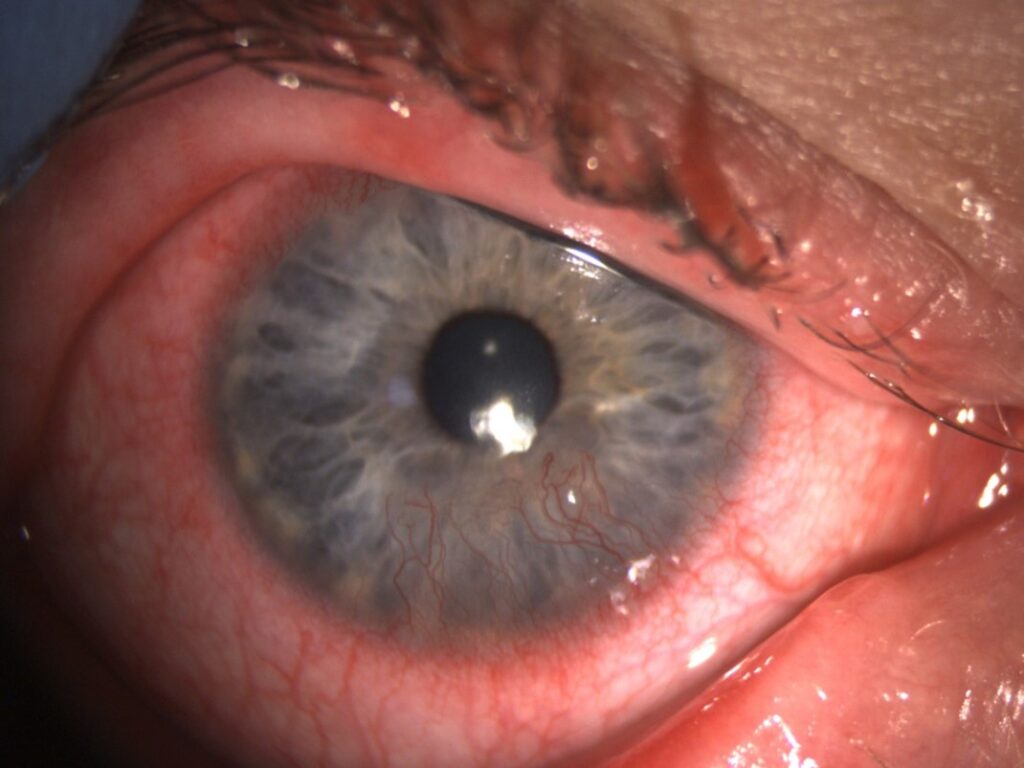
Maintenance treatment with allogenic tears proved beneficial in that the patients ocular surface improved. Right eye (RE) visual acuity of 6/9 and left eye (LE) visual acuity of 6/60. The patient remained stable for around 12 months then presented with peripheral ulcerative keratitis in the right eye. (Figure 2) This was again treated with oral prednisolone 40mg with a tapering dose over two months. The patient was also a steroid responder and developed raised pressure 33mmHg in his right eye. In order to prevent progressive inflammation and vascularisation in his better seeing eye, further systemic immunotherapy options in addition to oral steroids were considered.
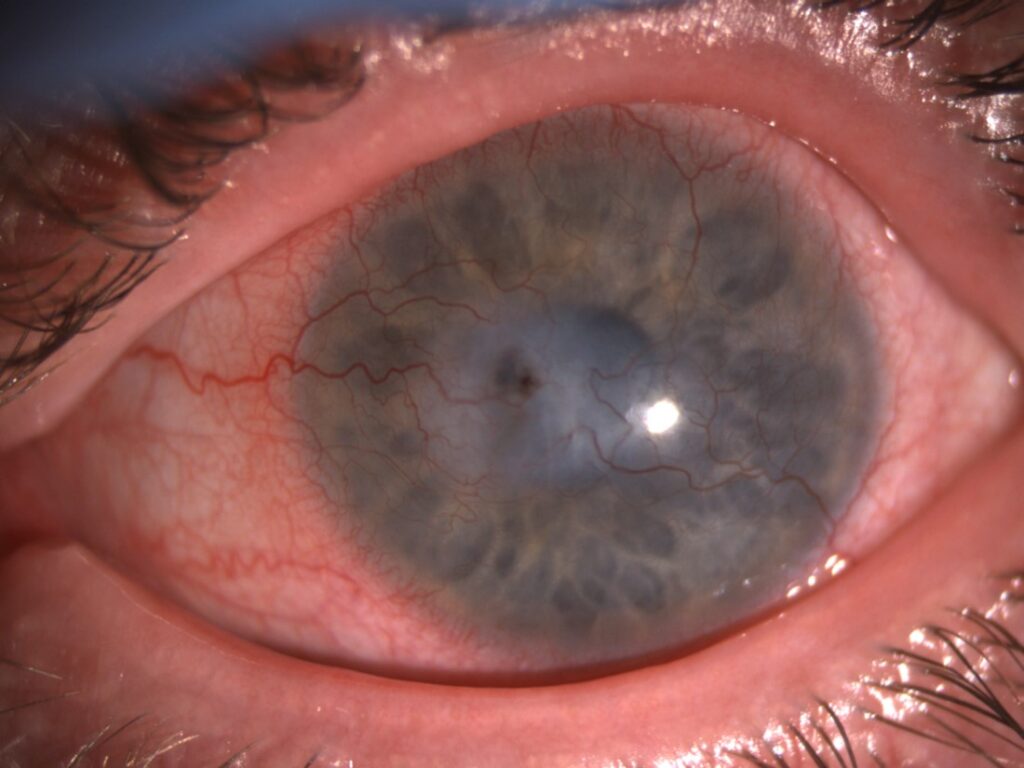
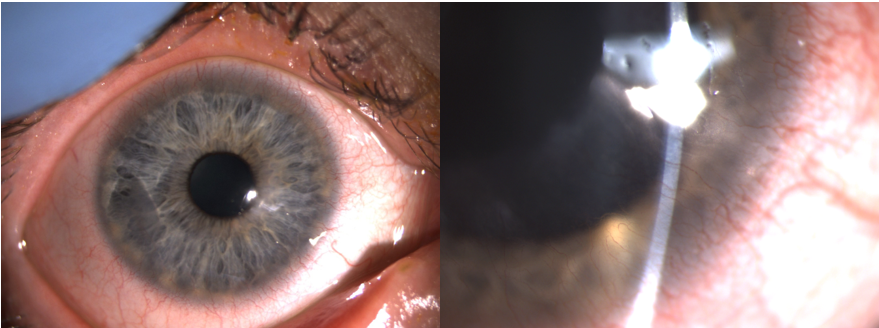
After discussion with the immunology team, with informed consent it was agreed to commence Anakinra (Interleukin-1 Receptor antagonist) 100mg daily by subcutaneous injection. Six months after starting Anakinra his ocular surface remains stable with an acuity of 6/9 right eye and counting fingers left eye. (Figures 3 & 4) In addition to Anakinra he used blood derived allogeneic tears 6 times per day and preservative free dexamethasone 0.1% once per day to both eyes. There is no ocular surface inflammation. Corneal vascularisation is inactive with regression in the right eye, maintaining a clear visual axis.
Discussion
It is uncommon for patients with CGD to present with such severe ocular surface inflammation. The cause of the ocular inflammation seemed to be related to the severe acne which affected the eyelid margins. Acne is both common and severe in patients with CGD. The Immunology MDT speculated that the ‘frustrated neutrophil’ mechanism would likely account for this patient’s severe ocular surface disease. The theory would be that CGD neutrophils cannot eradicate ingested organisms well but can still secrete cytokines and do so excessively in the face ongoing stimulation or infection. As this is predominately IL1 driven, the suggestion in corroboration with Immunology was to initiate Anakinra, an intrleukin-1 receptor antagonist.
Conclusion
This case focused in on a young male patient with X linked CGD presenting with ocular manifestations. In this context, Anakinra, a IL-1 receptor antagonist immunosuppressant, is a novel treatment that may be considered in such cases. Our patient has made good clinical progress with this treatment regimen. However, despite documented ocular manifestations of CGD, there is very few documented cases of such severe ocular disease secondary to CGD managed in this unique manner.
Latest Articles



HCP Popup
Are you a healthcare or eye care professional?
The information contained on this website is provided exclusively for healthcare and eye care professionals and is not intended for patients.
Click ‘Yes’ below to confirm that you are a healthcare professional and agree to the terms of use.
If you select ‘No’, you will be redirected to scopeeyecare.com
This will close in 0 seconds